The known: The carbon footprint of operating rooms is considerable, partly because some volatile anaesthetic gases are potent greenhouse gases. Reducing their use is important for achieving Net Zero health care targets.
The new: During 2002–2022, the main anaesthetic gas contributor to greenhouse gas emissions was desflurane. Rapid reductions in its use since 2017 were associated with large reductions in the overall emissions rate associated with anaesthetic gases in Australia.
The implications: Greater awareness of the global warming potential of desflurane has led to its reduced use in anaesthesia in Australia. Continuing to reduce its use could further limit the carbon footprint of anaesthesia.
To contribute to achieving global and national carbon emission reduction targets, health systems must reduce their carbon footprint. Health care accounts for about 4% of total greenhouse gas emissions.1 Operating rooms are among the major contributors;2 in two North American hospitals, for example, volatile anaesthetic gases contributed more than half the operating rooms greenhouse gas emissions, compared with 5% at a United Kingdom hospital that had eliminated desflurane.3 Reducing the use of volatile anaesthetic gases is therefore one measure for reducing the carbon footprint of clinical care.4,5
Three volatile anaesthetics are currently used in Australia: isoflurane, desflurane, and sevoflurane.6 Isoflurane was introduced in the early 1980s,7 sevoflurane and desflurane were approved for medical use in Australia in the 1990s.8,9 These anaesthetic gases were reportedly associated with less airway irritation, more rapid waking, and greater safety at deep anaesthesia levels than older alternatives.10
Global warming potential is often used in national and international agreements for quantifying the potential contribution of greenhouse gases to climate change.11 The carbon dioxide equivalent (CO2e) is a measure used to compare greenhouse gas emissions with respect to their global warming potential; it is determined by converting the amount of the gas to an equivalent amount of carbon dioxide.12 The 100‐year global warming potential of desflurane (2590 CO2e) is substantially higher than that of sevoflurane (144 CO2e) or isoflurane (539 CO2e),11 and phasing out the use of desflurane could reduce the overall carbon footprint of anaesthetic gases.13 As less polluting and less expensive but clinically equivalent alternatives are available,14 desflurane use is being reduced in some regions, including Europe, but not others, such as Asia.15,16
Desflurane has been removed from public hospital medicines formularies in New South Wales17 and Western Australia.18 However, 49% of Australian hospitals are private hospitals, and they perform 68% of elective surgery procedures;19 public hospital medicines formularies do not apply to these hospitals. Other options for reducing emissions and the costs associated with anaesthesia are low flow fresh gas delivery of anaesthetic gases, which reduces the amount of gas needed,11,20 and total intravenous anaesthesia using propofol.21
Information about CO2e emissions associated with anaesthesia in Australia is limited, despite their importance for the carbon footprint of health care. We therefore examined the use of anaesthetic gases and their associated CO2e emissions in Australian health care during 2002–2022. We provide a descriptive overview of changes in CO2e emissions associated with desflurane, sevoflurane, and isoflurane use, overall and by state or territory and hospital type.
Methods
We undertook a retrospective analysis of purchasing data for all Australian public and private hospitals, 1 January 2002 – 31 December 2022. We report our study in accordance with the Reporting of studies Conducted using Observational Routinely‐collected Data (RECORD) guidelines.22
Data source
Complete desflurane, sevoflurane, and isoflurane purchasing records were obtained from IQVIA (https://www.iqvia.com), a private data agency that collects data on the supply and sale of pharmaceuticals worldwide. The dataset covered all anaesthetic gas purchases (number of units and volume) in Australia by hospital, hospital type, hospital location, and month of purchase during 2002–2022. All purchases were converted to standard sizes (desflurane: 240 mL bottles; isoflurane, sevoflurane: 250 mL bottles). We validated the IQVIA dataset for desflurane and sevoflurane by comparing it with datasets supplied by the purchasing departments of two hospitals in Victoria and five in New South Wales.
Outcomes
We calculated the following CO2e emission rates for each anaesthetic gas, using published 100‐year global warming potential values:11 0.91 t/unit for desflurane, 0.20 t/unit for isoflurane, and 0.05 t/unit for sevoflurane. We report the CO2e emissions in absolute amounts per year and as emission rates per 100 000 population, based on Australian Bureau of Statistics population data for each study year and state/territory.23
Variables
We categorised all purchasing sites as public or private hospitals. Three (of 566) purchasing sites were buying groups that supplied more than one clinical site; the three were categorised according to the hospital type they supplied (two private, one public). We grouped hospital purchasing data by state and territory. To avoid identifying individual hospitals in analyses by state/territory, data were combined for the pairs Australian Capital Territory and New South Wales, South Australia and the Northern Territory, and Victoria and Tasmania.
Data analysis
We determined the total number of anaesthetic gas units purchased (by type) each year. We aggregated carbon footprints for each of the three gases and report their emissions by year and gas type. We also report emissions by state/territory and hospital type, and calculated emission rates per 100 000 population. Using joinpoint regression analysis (Joinpoint Trend Analysis Software 5.2.0) we estimated changes in total emissions and emission rates, overall and by state/territory, gas type, and hospital type, as annual percentage change (APC) between joinpoints (with 95% confidence interval, CI). Joinpoint regression, a form of segmented regression, is useful for analysing descriptive time series datasets with the aim of identifying timepoints of significant changes in trend.24 All other analyses and visualisations were performed in Excel (Microsoft).
Ethics approval
We did not seek formal research ethics approval for our analysis of purchasing data. Access to the data and permission to publish results based on them was granted by IQVIA as the data custodian.
Results
Total emissions for the three anaesthetic gases increased from 14 550 t CO2e in 2002 to 75 152 t CO2e in 2013 (plateau: 2008–2017), then declined to 21 802 t CO2e in 2022 (Box 1, A). The overall emissions rate increased from 74 t CO2e per 100 000 population in 2002 to 328 t CO2e per 100 000 population in 2012, then declined to 83 t CO2e per 100 000 population in 2022. The increase in the emissions rate was most marked during 2002–2004 (APC, 51%; 95% CI, 38–62%). The emissions rate slowly declined between 2008 and 2017, then fell rapidly during 2017–2022 (APC, –21%; 95% CI, –23% to –20%) (Box 1, B; Supporting Information, table 2).
Desflurane provided the largest proportion of total emissions from anaesthetic gases during 2002–2022: 33% in 2002, 88% in 2013, and 68% in 2022 (Box 1, A). The CO2e emission rate for desflurane rose most rapidly during 2002–2004 (APC, 120%; 95% CI, 84–148%) and declined during 2017–2022 (APC, –23%; 95% CI, –29% to –20%) (Supporting Information, table 2). The emissions rate for sevoflurane was below 50 t CO2e per 100 000 population throughout 2002–2022; the rate for isoflurane was below 10 t CO2e per 100 000 population during 2007–2022 (Box 1, B).
More units of sevoflurane than of desflurane or isoflurane were purchased each year throughout 2002–2022; in 2013, the peak year for desflurane purchasing (72 851 units), 153 075 units of sevoflurane were purchased. Isoflurane purchasing continuously declined from 24 692 units in 2002 to 785 units in 2022 (Supporting Information, figure 1).
Anaesthetic gas‐related emission rates, by state and territory
Mean emission rates per 100 000 population during 2002–2022 were highest for South Australia/Northern Territory (276 t CO2e per year) and Western Australia (258 t CO2e per year), and lowest for Victoria/Tasmania (196 t CO2e per year). The peak emission rate in South Australia/Northern Territory was 415 t CO2e per 100 000 population in 2013; in Victoria/Tasmania, the peak was 278 t CO2e per 100 000 population in 2009. Patterns of change in emission rates were similar for all states and territories: they increased during 2002–2008 in New South Wales/Australian Capital Territory, Queensland, and Victoria/Tasmania, during 2002–2013 in South Australia/Northern Territory, and during 2002–2016 in Western Australia. Emissions declined during 2008–2022 in New South Wales/Australian Capital Territory and Victoria/Tasmania, during 2013–2022 in South Australia/Northern Territory, and during 2016–2022 in Queensland and Western Australia (Box 2). The lowest estimated emission rate was the 2022 value for Western Australia (48 t CO2e per 100 000 population; 2019–2022: APC, –36%; 95% CI, –44% to –33%) (Supporting Information, table 2).
Anaesthetic gas‐related emission rates, by hospital type
Desflurane was associated with a larger proportion of total emissions from anaesthetic gases than sevoflurane throughout 2002–2022 in both public and private hospitals, and the desflurane emissions rate was higher for private than public hospitals. In public hospitals, the desflurane emissions rate increased from 10 t CO2e per 100 000 population in 2002 to 130 t CO2e per 100 000 population in 2009, then declined during 2009–2018 (APC, –8%; 95% CI, –10% to –5%) and more rapidly during 2018–2022 to 7 t CO2e per 100 000 population (APC, –43%; 95% CI, –48% to –37%). In private hospitals, the desflurane emissions rate increased from 14 t CO2e per 100 000 population in 2002 to 170 t CO2e per 100 000 population in 2015; it declined from 154 t CO2e per 100 000 population in 2017 to 49 t CO2e per 100 000 population in 2022 (APC, –20%; 95% CI, –24% to –17%) (Box 3; Supporting Information, table 2). Changes in desflurane emission rates for public and private hospitals were similar in all states and territories (Supporting Information, figure 2A).
The sevoflurane emissions rate was relatively constant during 2002–2022; the rate was slightly higher in public (12–20 t CO2e per 100 000 population) than private hospitals (12–16 t CO2e per 100 000 population) (Box 3). In some years, sevoflurane emission rates were higher for private than public hospitals in Queensland and Western Australia (Supporting Information, figure 2B).
Discussion
We report the first study of national changes in emissions related to volatile anaesthetic gases in Australia, based on a near complete dataset for a 21‐year period. Reporting emission rates per 100 000 population directly adjusted our results for significant changes in the population number during the past 21 years, and indirectly for changes in surgical volume. We found that greenhouse gas emissions associated with the three anaesthetic gases increased during 2002–2008, then declined during 2017–2022. Desflurane was not only the major contributor to volatile anaesthesia‐related emissions; desflurane emissions alone would have contributed 0.18% of estimated total health care emissions in Australia during 2014–15 (35 772 kt).25 Sevoflurane was the most purchased anaesthetic gas in Australia during 2002–2022, but the emissions impact was lower than that of desflurane because of the lower emissions per unit rate. Isoflurane contributed least to emissions because its use in medical practice is very limited. Emission rates by population were lowest in Victoria/Tasmania and highest in South Australia/Northern Territory. The steepest fall in the desflurane emissions rate was in Western Australia, where the overall anaesthetic gas emissions rate was lowest by 2022. Anaesthetic gas‐related emission rates declined in both private and public hospitals during 2017–2022, particularly the desflurane emissions rate, the decline in which commenced earlier and was more rapid in public than in private hospitals.
As awareness of the harmful climate impact of desflurane and the availability of safe and clinically appropriate alternatives increases,21 professional bodies and anaesthetists have called for removing it from use, including the Australian and New Zealand College of Anaesthetists26 and Trainee‐led Research and Audit in Anaesthesia for Sustainable Healthcare (TRA2SH).27 Western Australia and New South Wales have removed desflurane from pharmaceutical formularies,17,18 but these bans apply only to public hospitals, and most elective surgery procedures are performed in private hospitals.28 Desflurane use has declined in private hospitals without legislative measures, albeit at a slower pace than in public hospitals, perhaps because of private hospital group initiatives, such as the Ramsay Health Care Greener Theatre program, which promotes low carbon anaesthetic choice and low flow anaesthesia.29
Reasons for using desflurane include patient (eg, high body mass index), anaesthetic (eg, sevoflurane viewed as slow or potentially dangerous at low flow), surgical (eg, long duration surgery), and organisational factors (eg, established institutional practice).30 Lack of awareness of the environmental harms, clinician preferences, promotion of desflurane, and ease of access also influence clinicians’ choosing desflurane, especially as the higher cost of the agent is not directly borne by the provider or patient.30 However, a range of interventions have successfully reduced the use of desflurane, including education and awareness campaigns,20,31 forming green environmental staff groups,32 and environmental modifications,33 such as removing desflurane vaporisers from operating rooms,34 providing equipment and training in total intravenous anaesthesia,30 and promoting low flow anaesthetic practices.35,36
Educational campaigns about the environmental impact of anaesthesia, particularly desflurane, have led to changes in clinical practice.31,32 For example, emissions can be significantly reduced by low flow anaesthesia.37 The Australian and New Zealand College of Anaesthetists Environmental Sustainability Audit tool specifically refers to the emission reductions of low flow anaesthesia, which reduces the fresh carrier gas flow in a closed circuit system, conserving gas by returning at least half the exhaled gas mixture to the patient after removing carbon dioxide.38 Increased awareness through the efforts of individual clinicians, followed by more widespread and sustained educational and training initiatives, possibly initiated and now sustain the decline in anaesthetic gas emissions we have reported.
Implications for policy, practice, and research
Given the carbon footprint of desflurane, reducing or eliminating its use has major implications for the carbon footprint of anaesthesia in Australia. Anaesthetic agents with smaller carbon footprints, such as sevoflurane and intravenous propofol, are already promoted by professional organisations, in line with the second objective of the National Health and Climate Strategy (health system decarbonisation).39
As the legislated removal of desflurane from public hospitals in Western Australia and New South Wales has only recently come into effect, further monitoring of emissions will be informative. Given the slower decline in desflurane use in private hospitals, identifying and overcoming barriers to reducing its use are needed. One barrier may be clinicians’ perceptions of more rapid recovery times with desflurane.30 This perception may be especially influential in private hospitals, which undertake a large proportion of scheduled and elective surgery procedures in Australia, as more rapid recovery could facilitate moving more patients through surgery and recovery.28 However, evidence is increasing that differences between desflurane and other anaesthetic agents, such as sevoflurane and intravenous propofol, with regard to patient recovery and anaesthetic‐related respiratory complications are negligible.21,30 Desflurane use related to these factors could therefore be reduced by targeted education and awareness campaigns. Leadership by private hospitals is needed, as governments are less able to influence the anaesthetic formularies of private hospitals. The Australian Commission on Safety and Quality in Health Care Environmental Sustainability and Climate Resilience Healthcare Module, an action framework for optimising the quality and safety of care in public and private health services while reducing the contribution of health care to climate change,40 will include such measures in several private health care facilities (to be published in late 2025).
Different procurement structures in states and territories complicate regulation. The Australian National Climate and Health Unit can assist state and territory bodies with developing plans, establishing targets, and coordinating change for reducing anaesthetic gas use. The recently formed sustainable health care units in Western Australia and New South Wales could also play roles. Establishing similar units in other states and territories could assist with developing further interventions, enabling clinicians and key decision makers to decarbonise all aspects of anaesthesia.
Limitations
Suppliers may sometimes not use traditional pharmaceutical wholesalers, and these purchases would not be captured in IQVIA data. This, however, would be infrequent. While we would have preferred a denominator for calculating emission rates that accounted directly for changes in surgery volume and duration (ie, per 1000 operations or 1000 operation‐hours), obtaining the required data from every hospital for each year of the 21‐year period was not possible. Additionally, as individual patient data were unavailable, our rates could not be age‐standardised. However, our population denominator is probably correlated with surgery volume and therefore accounts, if incompletely, for changes in surgical volume and practices. We could not take into account changes in surgical volume not correlated with population growth, such as those caused by elective surgery restrictions during the coronavirus disease 2019 (COVID‐19) pandemic.
Conclusion
Greenhouse gas emissions attributable to anaesthetic gases used in Australian hospitals increased significantly during 2002–2008. Desflurane was responsible for the largest proportion of these emissions because of its large carbon footprint, although sevoflurane was the most purchased anaesthetic gas throughout 2002–2022. Patterns of changes in anaesthetic gas use were similar in all states and territories. The desflurane‐related emissions rate declined earlier in public than private hospitals. Reducing the use of desflurane and anaesthetic gases more broadly will advance the decarbonisation of clinical practice in Australian health care.
Box 1 – Total CO2e emissions and population carbon dioxide equivalent (CO2e) emission rates for anaesthetic gases, Australia, 2002–2022, overall and by anaesthetic gas*
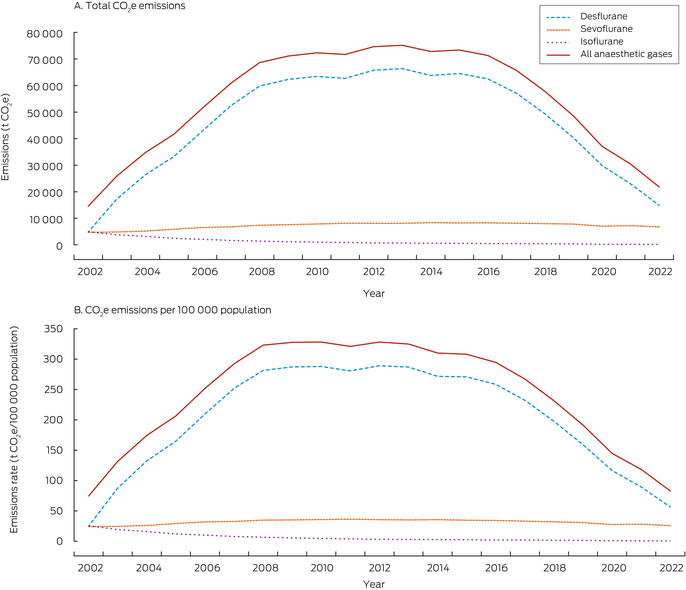
The data underlying this graph are included in the Supporting Information, table 1.
Box 2 – Population carbon dioxide equivalent (CO2e) emission rates for anaesthetic gases, Australia, 2002–2022, by state and territory*
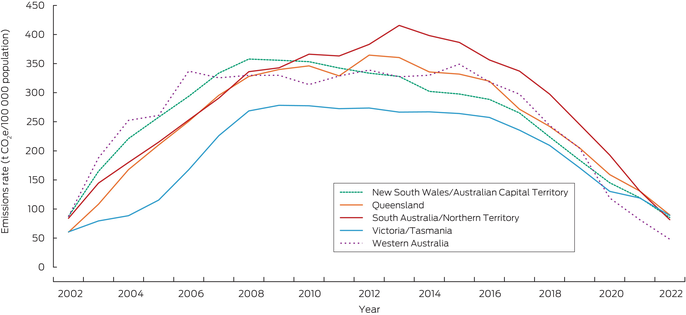
The data underlying this graph are included in the Supporting Information, table 3.
Box 3 – Population carbon dioxide equivalent (CO2e) emission rates for desflurane and sevoflurane, Australia, 2002–2022, by hospital type*
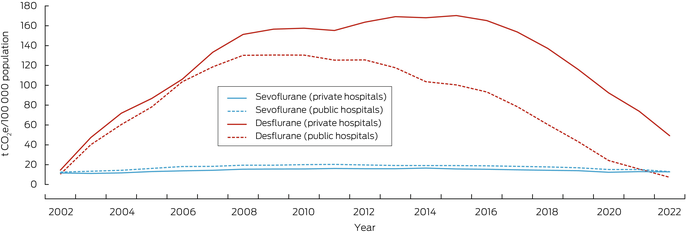
The data underlying this graph are included in the Supporting Information, table 4.
Received 12 December 2024, accepted 13 May 2025
- Krista Verlis1
- Jessica F Davies2,3
- Forbes McGain3,4
- Hayden Burch2,3
- Alexandra L Barratt1
- Luise Kazda1,5
- 1 Sydney School of Public Health, the University of Sydney, Sydney, NSW
- 2 Austin Health, Melbourne, VIC
- 3 The University of Melbourne, Melbourne, VIC
- 4 Western Health, Melbourne, VIC
- 5 Health Research Institute, University of Canberra, Canberra, ACT
Open access:
Open access publishing facilitated by the University of Sydney, as part of the Wiley – the University of Sydney agreement via the Council of Australian University Librarians.
Data Sharing:
The purchasing data we analysed are not publicly available and cannot be shared by the authors, as we do not have permission from the data custodian to do so.
Krista Verlis and Luise Kazda are supported by the Healthy Environments And Lives (HEAL) National Research Network, which receives funding from the National Health and Medical Research Council (NHMRC) Special Initiative in Human Health and Environmental Change (grant no. 2008937). Jess Davies received a research scholarship from the Australian and New Zealand College of Anaesthetists (ANZCA). These funds were used to help pay for the IQVIA data. The funding sources were not involved in planning, writing or publishing this work, nor did they have any role in the research.
Forbes McGain receives royalties from Medihood for the co‐invented, patented McMonty hood.
Authors’ contributions:
Funding acquisition: Krista Verlis, Luise Kazda, Jess Davies, Alexandra Barratt. Conceptualisation: Krista Verlis, Luise Kazda, Jess Davies, Alexandra Barratt. Data curation: Krista Verlis, Luise Kazda. Formal analysis: Krista Verlis, Luise Kazda, Forbes McGain. Methodology: Krista Verlis, Luise Kazda, Jess Davies, Forbes McGain, Hayden Burch, Alexandra Barratt. Project administration: Krista Verlis, Luise Kazda, Alexandra Barratt. Supervision: Luise Kazda, Alexandra Barratt. Visualisation: Krista Verlis, Luise Kazda. Writing (original draft): Krista Verlis. Writing (review and editing): Krista Verlis, Luise Kazda, Jess Davies, Forbes McGain, Hayden Burch, Alexandra Barratt.
- 1. Rodríguez‐Jiménez L, Romero‐Martín M, Spruell T, et al. The carbon footprint of healthcare settings: a systematic review. J Adv Nurs 2023; 79: 2830‐2844.
- 2. Varughese S, Ahmed R. Environmental and occupational considerations of anesthesia: a narrative review and update. Anesth Analg 2021; 133: 826‐835.
- 3. MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health 2017; 1: e381‐e388.
- 4. Yasny JS, White J. Environmental implications of anesthetic gases. Anesth Prog 2012; 59: 154‐158.
- 5. Pauchard JC, Hafiani EM, Pons S, et al. Guidelines for reducing the environmental impact of general anaesthesia. Anaesth Crit Care Pain Med 2023; 42: 101291.
- 6. McGain F, Bishop JR, Elliot‐Jones LM, et al. A survey of the choice of general anaesthetic agents in Australia and New Zealand. Anaesth Intensive Care 2019; 47: 235‐241.
- 7. McDonald J. 1974–1983: a decade of advances. Australian Society of Anaesthetists. Undated. https://asa.org.au/1974‐1983‐a‐decade‐of‐advances (viewed Oct 2024).
- 8. Therapeutic Goods Administration (Australian Department of Health and Aged Care). SEVORANE sevoflurane anaesthetic inhalation bottle (ARTG ID 51919). 4 Jan 1996. https://www.tga.gov.au/resources/artg/51919 (viewed Oct 2024).
- 9. Therapeutic Goods Administration (Australian Department of Health and Aged Care). SUPRANE desflurane 1g/g inhalation USP bottle (ARTG ID 60909). 20 Aug 1997. https://www.tga.gov.au/resources/artg/60909 (viewed Oct 2024).
- 10. Patel SS, Goa KL. Sevoflurane: a review of its pharmacodynamic and pharmacokinetic properties and its clinical use in general anaesthesia. Drugs 1996; 51: 658‐700.
- 11. Sulbaek Andersen MP, Nielsen OJ, Sherman JD. Assessing the potential climate impact of anaesthetic gases. Lancet Planet Health 2023; 7: e622‐e629.
- 12. Eurostat. Carbon dioxide equivalent. In: European Environmental Agency, Glossary. 10 Aug 2023. https://ec.europa.eu/eurostat/statistics‐explained/index.php?title=Glossary: Carbon_dioxide_equivalent (viewed Jan 2025).
- 13. Sulbaek Andersen MP, Sander SP, Nielsen OJ, et al. Inhalation anaesthetics and climate change. Br J Anaesth 2010; 105: 760‐766.
- 14. Devlin‐Hegedus J, McGain F, Harris R, Sherman JD. Action guidance for addressing pollution from inhalational anaesthetics. Anaesthesia 2022; 77: 1023‐1029.
- 15. Vollmer MK, Rhee TS, Rigby M, et al. Modern inhalation anesthetics: potent greenhouse gases in the global atmosphere. Geophys Res Lett 2015; 42: 1606‐1611.
- 16. Hu EP, Yap A, Davies JF, et al. Global practices in desflurane use. Br J Anaesth 2023; 133: 1484‐1486.
- 17. NSW Health. Environmental impact of desflurane. 28 Feb 2024. https://www.health.nsw.gov.au/netzero/Pages/environmental‐impact‐desflurane.aspx (viewed Oct 2024).
- 18. Department of Health (Western Australia). Surgery switches to “low carbon”: WA Health takes the knife to high‐emissions anaesthetic [media release]. 5 Oct 2023. https://www.health.wa.gov.au/Media‐releases/2023/October/WA‐Health‐takes‐the‐knife‐to‐high‐emissions‐anaesthetic (viewed Oct 2024).
- 19. Australian Private Hospital Association. Federal budget submission 2019–20. 24 Aug 2020. https://treasury.gov.au/sites/default/files/2020‐09/115786_AUSTRALIAN_PRIVATE_HOSPITALS_ASSOCIATION_‐_SUBMISSION_2.pdf (viewed Oct 2024).
- 20. Wyssusek K, Chan KL, Eames G, Whately Y. Greenhouse gas reduction in anaesthesia practice: a departmental environmental strategy. BMJ Open Qual 2022; 11: e001867.
- 21. Schraag S, Pradelli L, Alsaleh AJO, et al. Propofol vs. inhalational agents to maintain general anaesthesia in ambulatory and in‐patient surgery: a systematic review and meta‐analysis. BMC Anesthesiol 2018; 18: 162.
- 22. Benchimol EI, Smeeth L, Guttmann A, et al; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely‐collected health Data (RECORD) statement. PLoS Med 2015; 12: e1001885.
- 23. Australian Bureau of Statistics. National, state and territory population, December 2024. 19 June 2025. https://www.abs.gov.au/statistics/people/population/national‐state‐and‐territory‐population/latest‐release (viewed Sept 2024).
- 24. Kim HJ, Chen HS, Byrne J, et al. Twenty years since Joinpoint 1.0: two major enhancements, their justification, and impact. Stat Med 2022; 41: 3102‐3130.
- 25. Malik A, Lenzen M, McAlister S, McGain F. The carbon footprint of Australian health care. Lancet Planet Health 2018; 2: e27‐e35.
- 26. Australian and New Zealand College of Anaesthetists. ANZCA statement on desflurane. Nov 2024. https://www.anzca.edu.au/resources/environmental‐sustainability/anzca‐statement‐on‐desflurane‐2024.pdf (viewed Aug 2024).
- 27. Davies JF, Seglenieks R, Cameron R, et al. Operation clean up: a model for eco‐leadership and sustainability implementation. Anaesth Intensive Care 2023; 51: 88‐95.
- 28. Australian Institute of Health and Welfare. Hospitals at a glance (here: table 3). Updated 13 May 2025. https://www.aihw.gov.au/reports/hospitals/australias‐hospitals‐at‐a‐glance (viewed Aug 2025).
- 29. Ramsay Health Care. Caring for our planet. Undated. https://www.ramsayhealth.com/en/sustainability/caring‐for‐our‐planet (viewed Sept 2024).
- 30. Ang KS, Low ZK, Ng BSW, Poh PK. Developing a quality improvement project to tackle the desflurane problem. BMJ Open Qual 2023; 12: 002132.
- 31. Zuegge KL, Bunsen SK, Volz LM, et al. Provider education and vaporizer labeling lead to reduced anesthetic agent purchasing with cost savings and reduced greenhouse gas emissions. Anesth Analg 2019; 128: e97‐e99.
- 32. Chambrin C, de Souza S, Gariel C, et al. Association between anesthesia provider education and carbon footprint related to the use of inhaled halogenated anesthetics. Anesth Analg 2023; 136: 101‐110.
- 33. Hansen EE, Chiem JL, Righter‐Foss K, et al. Project SPRUCE: Saving Our Planet by Reducing Carbon Emissions, a pediatric anesthesia sustainability quality improvement initiative. Anesth Analg 2023; 137: 98‐107.
- 34. Richter H, Weixler S, Schuster M. Der CO2‐Fußabdruck der Anästhesie. Wie die Wahl volatiler Anästhetika die CO2‐Emissionen einer anästhesiologischen Klinik beeinflusst. Anästh Intensivmed 2020; 61: 154‐161.
- 35. Nordin EJ, Dugan SM, Kusters AC, et al. How an audit‐and‐feedback‐based educational program contributed to a reduction in environmentally harmful waste anesthetic gases among anesthesiology residents. J Grad Med Educ 2024; 16: 175‐181.
- 36. Olmos AV, Robinowitz D, Feiner JR, et al. Reducing volatile anesthetic waste using a commercial electronic health record clinical decision support tool to lower fresh gas flows. Anesth Analg 2023; 136: 327‐337.
- 37. McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth 2020; 125: 690‐692.
- 38. McGain F, Ma SC, Burrell RH, et al. Why be sustainable? The Australian and New Zealand College of Anaesthetists professional document PS64: Statement on environmental sustainability in anaesthesia and pain medicine practice and its accompanying background paper. Anaesth Intensive Care 2019; 47: 413‐422.
- 39. Australian Department of Health and Aged Care. National health and climate strategy. 3 Dec 2023. https://www.health.gov.au/resources/publications/national‐health‐and‐climate‐strategy?language=en (viewed July 2024).
- 40. Australian Commission on Safety and Quality in Healthcare. Environmental sustainability and climate resilience healthcare module. Updated 8 Nov 2024. https://www.safetyandquality.gov.au/standards/environmental‐sustainability‐and‐climate‐resilience‐healthcare‐module (viewed Oct 2024).






Abstract
Objectives: To assess changes in greenhouse gas emission rates associated with the use of anaesthetic gases (desflurane, sevoflurane, and isoflurane) in Australian health care during 2002–2022, overall and by state or territory and hospital type.
Study design: Retrospective descriptive analysis of IQVIA anaesthetic gases purchasing data.
Setting: All Australian public and private hospitals, 1 January 2002 – 31 December 2022.
Main outcome measures: Absolute carbon dioxide equivalent (CO2e) emissions and CO2e emissions rate per 100 000 population by gas and year, overall and by state/territory and hospital type (public or private).
Results: The overall emissions rate increased from 74 t CO2e per 100 000 population in 2002 to 328 t CO2e per 100 000 population in 2012, most rapidly during 2002–2004 (annual percentage change [APC], 51%; 95% confidence interval [CI], 38–62%). The rate then declined to 83 t CO2e per 100 000 population in 2022, most rapidly during 2017–2022 (APC, –21%; 95% CI, –23% to –20%). Patterns of emissions rate change were similar for all states and territories. More units of sevoflurane than of desflurane or isoflurane were purchased each year throughout 2002–2022, but desflurane provided the largest proportion of total emissions from anaesthetic gases during 2002–2022: 33% in 2002, 88% in 2013, and 68% in 2022. Mean emission rates per 100 000 population during 2002–2022 were highest for South Australia/Northern Territory (276 t CO2e per year) and lowest for Victoria/Tasmania (196 t CO2e per year). The desflurane emissions rate was consistently higher for private than public hospitals; it declined for public hospitals during 2009–2018 (APC, –8%; 95% CI, –10% to –5%) and 2018–2022 (APC, –43%; 95% CI, –48% to –37%), but for private hospitals only during 2017–2022 (APC, –20%; 95% CI, –24% to –17%).
Conclusions: In Australia, the CO2e emissions rate for anaesthetic gases increased during 2002–2008 but declined during 2017–2022, at first primarily in public hospitals. Continuing to reduce the use of anaesthetic gases, particularly desflurane, will advance the decarbonisation of clinical practice in Australian health care.