As Australia emerges from the coronavirus disease 2019 (COVID‐19) pandemic, and H5 avian influenza approaches global spread, it is instructive to reflect on past Australian pandemic experiences. This is underscored by the recent Australian Government's COVID‐19 Response Inquiry Report.1
Within just over a century Australia has been affected by five respiratory virus pandemics: four influenza pandemics and the recent coronavirus pandemic. The deadliest was the Spanish influenza pandemic (1918), followed by the moderately severe Asian (1957) and Hong Kong (1968) influenza pandemics, the mild influenza pandemic originating in North America (2009), and then the COVID‐19 pandemic (2020).
The Hong Kong influenza pandemic arose midway between the Spanish influenza and COVID‐19 pandemics, during the momentous events of the late 1960s. It spanned Vietnam War protests and Woodstock, and affected United States presidents and Apollo astronauts. However, there are relatively few published accounts of Australia's experiences. This article reviews historical literature and contemporaneous news reports to extract insights for future pandemic responses. This forgotten pandemic has some notable similarities and differences to Australian experiences of the Spanish influenza and COVID‐19 pandemics (Box 1).
Classification of influenza
Only type A viruses cause pandemic influenza, and they are defined by the two surface antigens haemagglutinin (H) and neuraminidase (N). Both undergo antigenic variation, which sustains virus epidemic potential, and serve as targets for the protective antibody response, with haemagglutinin being the major and more significant antigen. Pandemic influenza is associated with a virus possessing a novel haemagglutinin. Influenza A viruses were initially subtyped as A0, A1 and A2 (H0, H1 and H2) based on haemagglutination‐inhibition tests.
The revised 1971 World Health Organization nomenclature recognised distinct antigenic forms of neuraminidase, retrospectively designating the Hong Kong virus as A(H3N2) and its A2 predecessor as A(H2N2), with distinct haemagglutinin but shared neuraminidase. Genomic sequencing now supplements antigenic tests in characterising these viruses. Antigenic variants of the initial A(H3N2) virus continue to circulate alongside A(H1N1) and type B viruses and result in the highest rates of influenza‐related morbidity and mortality.2,3
Chronology of the pandemic
The Hong Kong influenza virus probably originated in China in early 1968 during the Cultural Revolution, with unclear reports of an epidemic involving Chinese cities including Wuhan, Shanghai and Guiyang.4 In July 1968, a respiratory illness outbreak was identified in Hong Kong, with about half a million cases reported by the end of that month.5
On 16 August 1968, the Hong Kong epidemic was attributed to an influenza virus significantly different from previous strains. Initial antigenic tests suggested a low level of relatedness to the pre‐existing A2 Asian influenza virus family, and it was referred to as a major variant of that virus.6 However, subsequent testing indicated a distinct haemagglutinin subtype.6,7 By the end of August 1968, the virus had spread to Singapore, Vietnam, Taiwan, the Philippines and Australia.5,8
In Australia, the 1968 winter seasonal influenza epidemic was notably severe in Sydney. In a newspaper report on 11 August 1968, Dr H Kramer (Director of the Institute of Clinical Pathology at Lidcombe) identified the cause as the Asian A2 strain,9 and Dr RW Lane (Director of the Commonwealth Serum Laboratories [CSL]) described it as “the worst outbreak since 1957”.9 Outbreaks of the Asian A2 virus were also recorded in Victoria,10 South Australia,11 and Western Australia, where the Premier, Deputy Premier and two state ministers were among those afflicted.12 The world's last isolation of Asian influenza is said to have occurred in Australia in August 1968.11,13
On 30 August 1968, Australia's first confirmation of Hong Kong influenza occurred when CSL isolated and identified the strain from a patient in the Northern Territory who had returned from Hong Kong.8 Around the same time, Dr Peter Arnold (a Sydney general practitioner based in Bellevue Hill) identified five cases that were confirmed as Hong Kong influenza via a collaboration with the Institute of Clinical Pathology. Four of these cases had returned from Bowral in New South Wales with reports of a “generalised outbreak of an influenza‐like illness at their hotel”.14 Curiously, the new Hong Kong influenza virus did not cause a significant epidemic wave in Australia in 1968.
During September and October 1968, there were 295 cases of Hong Kong influenza clinically diagnosed on board a cruise ship from Sydney as part of its voyage to Honolulu (United States), continental North America, Japan and Hong Kong. Dr BD Apthorp, who described the outbreak, reported the onset of illness was “identical in nearly every case”, with a headache, which patients frequently described as “it feels as if the top of my head is lifting off”. Despite these observations, only a small number of patients developed signs suggestive of pneumonia and the author did not report any deaths.15
In 1968, Australia had sovereign capacity to mass produce influenza vaccines at CSL. By November, it started to send 1.3 million Hong Kong influenza vaccine doses to Britain to help with the expected winter surge.16 CSL assumed the novel influenza virus would follow a conventional seasonal pattern and that Australia would not require vaccine for several months — a significant gamble by current standards given the unpredictable nature of other influenza pandemic outbreaks.17 Subsequently, CSL produced over 6 million vaccine doses in Australia for the 1969 winter.16,18
The first case in the US was identified in a soldier returning from Vietnam in early September 1968. Subsequent cases were detected in military bases in California, Hawaii and Alaska.19 During the US winter of 1968–69 the virus spread rapidly, affecting President Lyndon Johnson, Vice President Hubert Humphrey, and President‐elect Richard Nixon. Apollo 8 astronauts together with 1200 personnel at Cape Kennedy were vaccinated to reduce disruption to the following year's planned moon landing. The first wave of Hong Kong influenza in the US was declared over in February 1969 with more than 100 000 deaths.20 By mid‐1969, mass gatherings such as Woodstock and the Moratorium March (the largest anti‐war protest in US history) occurred without apparent mention of the pandemic.21
Unlike the US, much of the world experienced a delayed impact from Hong Kong influenza. As with Australia's experience in 1968, this has been attributed to population immunity from recent exposure to H2N2 Asian influenza and mediated by antibody to the shared N2 neuraminidase.13 Although outbreaks occurred in the United Kingdom and continental Europe during the northern winter of 1968–69, in contrast to the US, the illness was mostly reported as mild.13 Many northern hemisphere countries outside North America experienced their worst season during the following winter of 1969–70. In England and Wales, for example, all cause excess mortality in the 1969–70 pandemic season (77.0 per 100 000 population) was almost twice that of the previous season (43.0 per 100 000 population) even though the Hong Kong influenza virus had first arrived there in 1968.13
In Australia, where the delay was most pronounced, tracing the early epidemiology of the new virus was complicated by the contemporaneous occurrence of the last recorded epidemic of the Asian A2 (H2N2) subtype and the new Hong Kong virus. Initial labelling of the new virus as an A2 variant may also have influenced reporting. Like in the UK and other parts of Europe, the 1969 pandemic wave in Australia was relatively mild. The influenza mortality rate (17 per 100 000 population) was considerably lower than the rate during the A2 epidemic in 1968 (27 per 100 000 population).22 However, in New Guinea the impact of Hong Kong influenza in 1969 was devastating. There were at least 2000 deaths, with possibly as many as 10 000. The army and air force were called in to assist with the response, including 200 soldiers of the Pacific Islands Regiment.23
Again mirroring the European experience, 1970 was the worst year for Hong Kong influenza in Australia. Remarkably, two years after the virus first arrived, Australian mortality reached 64 per 100 000 population.13 This was the highest influenza mortality since the Asian influenza pandemic. The 1970 epidemic appears to have started in Queensland in June with outbreaks among Aboriginal and Torres Strait Islander peoples in Cape York and the Torres Strait, spreading to Brisbane and then the rest of Australia.24 The NSW Premier became sick with it, George Johnson (author of My brother Jack) died of it, schools battled staff illness and crowding in classes, and Melbourne's city mortuary became full.25,26,27,28 In an echo of the US experience, over 200 000 people attended anti‐war protests across the country from May to September 1970,29 without apparent mention of the pandemic.
Impact
Our review of local and international medical literature, and search of media print publications, found only limited descriptions of the epidemiology, public health and societal impact of Hong Kong influenza in Australia.
Hong Kong influenza established the classical 12‐month seasonal cycle, with peaks of varying severity in different years and locations. For Spanish influenza there were three waves within 12 months before adopting a seasonal pattern, whereas COVID‐19 was initially experienced as synchronous global waves every three months after the emergence of the Omicron variant. The determinants of seasonality for respiratory viruses are incompletely understood but may include host innate immunity, environmental and/or climatic factors, and season‐dependent human behaviour. In addition, not all respiratory viruses have a winter seasonality.30 Pre‐existing partial immunity from H2N2 Asian influenza likely played a significant role in the behaviour of Hong Kong influenza.
When comparing the severity of Hong Kong influenza and COVID‐19 pandemics in Australia, it is important to note that there were delays in the peak of both pandemics, and, by this time, vaccines against both viruses were available. In the case of Hong Kong influenza, this was most likely due to naturally acquired antineuraminidase immunity;13 for COVID‐19, it was most likely due to non‐pharmaceutical interventions. Based on around 6 million doses distributed for Hong Kong influenza and uncertainty around whether a single or double dose was administered, this resulted in a much lower vaccination rate than the more than 90% rate achieved for COVID‐19. It would, however, likely complement any naturally acquired immunity.
Excess mortality is a common measure of epidemic and pandemic severity.2,13,17 Retrospective assessment of excess mortality for Australia across two seasons of the Hong Kong influenza pandemic approaches that of COVID‐19 from 2020 to 2023 (87.3 v 91.4 per 100 000 population).13,31 However, a smaller proportion of young people died of COVID‐19 compared with Hong Kong influenza. About 30% of Hong Kong influenza deaths occurred in Australians under 65 years old,13 compared with about 11% of COVID‐19 deaths reported among Australians less than 70 years old.32
Of course, the impact of the COVID‐19 pandemic was much greater in countries that experienced widespread transmission before the availability of effective vaccines. For example, the excess death rate was about 4.5 times higher in the US than in Australia (408 v 91.4 per 100 000 population),33 second only to Spanish influenza in terms of pandemic mortality in the modern era.
We note with interest that early outbreaks on cruise ships departing Sydney were reported for both pandemics. Of 907 COVID‐19 cases diagnosed on the Ruby Princess, 29 died (case fatality rate of 3.2%).34 In contrast, Dr Apthorp reported no deaths among 295 Hong Kong influenza cases on the Sydney cruise ship in spring 1968.15
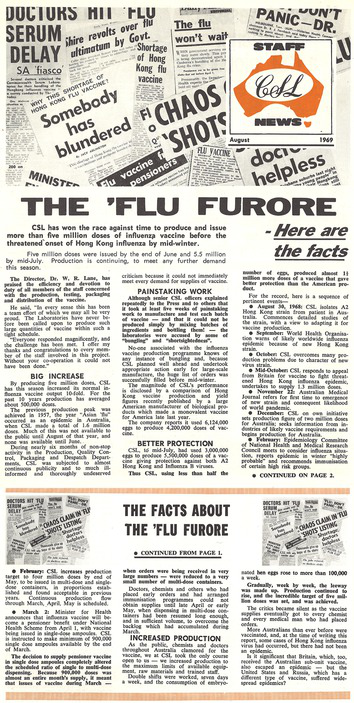
Compared with the response to COVID‐19, there were no border closures, contact tracing, lockdowns, social distancing, or school closures. Yet these measures allowed the Australian population to be vaccinated against COVID‐19 before infection was widespread. Both pandemics shared media and public concerns about vaccine supplies. The “flu furore” of early 1969 related to initial concerns over the availability of vaccines ahead of an expected epidemic of Hong Kong influenza that winter (Box 2).16 This illustrates the public's sensitivity to vaccine supply issues, which was also noted in the COVID‐19 Response Inquiry Report.1
Although vaccination is a cornerstone of pandemic response, one critical lesson from both the Hong Kong influenza and COVID‐19 experiences is that effective vaccination programs are shaped by timely deployment, public acceptance, and the unpredictable nature of viral spread. The Hong Kong influenza pandemic confirmed that even with vaccination and some degree of pre‐existing immunity, the timing and severity of outbreaks can be unpredictable (Box 3).
Australia's ability to manage future pandemics will depend not only on robust scientific and health care systems but also on fostering public trust and resilience, especially when balancing scientific uncertainty with the need for decisive action. By learning from these experiences, Australia can better anticipate and mitigate the complex social, economic and health impacts of future global health emergencies.
Box 1 – Search strategy
We searched the scientific literature using keywords including “Hong Kong flu”, “Hong Kong influenza”, “pandemic influenza”, “pandemic”, “influenza”, and “h3n2”. Additional searches, including subsearches of the above, used terms such as “Australia” and the names of its states and territories, as well as the years 1968–1974. Databases and sources searched included PubMed, Google Scholar, the Medical Journal of Australia, The British Medical Journal (BMJ), The Lancet, The New England Journal of Medicine, the Journal of the American Medical Association (JAMA), the Australian Institute of Health and Welfare, and archives of various Australian media outlets. In addition, we searched the National Archives of Australia and the National Library of Australia (Trove) for contemporaneous media reports, and conducted general internet searches.Box 3 – Lessons for future pandemic preparedness
- Any novel highly communicable viral respiratory pathogen is likely to arrive and spread in Australia within weeks of its first recognition overseas.
- A respiratory virus pandemic is experienced as a series of waves over a period of several years, but the severity and frequency of these waves may be impossible to predict.
- The ability to plan a specific pandemic response is limited without advance knowledge of the virulence and behaviour of a novel pathogen.
- Secure vaccine supply is a priority as uncertainty creates significant community concern.
- There was a notable difference between the public health response to the Hong Kong influenza and coronavirus disease 2019 (COVID‐19) pandemics. The response to the next pandemic is likely to be influenced by factors including the pathogen's behaviour, vaccine supply, political environment, media, and community risk perception.
Provenance: Not commissioned; externally peer reviewed.
- 1. Australian Government Department of the Prime Minister and Cabinet. COVID‐19 Response Inquiry Report. Canberra: Commonwealth of Australia, 2024. https://www.pmc.gov.au/resources/covid‐19‐response‐inquiry‐report (viewed Oct 2024).
- 2. Simonsen L. The global impact of influenza on morbidity and mortality. Vaccine 1999 (Suppl): S3‐S10.
- 3. Tekin S, Keske S, Alan S, et al. Predictors of fatality in influenza A virus subtype infections among inpatients in the 2015–2016 season. Int J Infect Dis 2019; 81: 6‐9.
- 4. The “Hong Kong flu” began in Red China. The New York Times 1968; 15 Dec. https://www.nytimes.com/1968/12/15/archives/the‐hong‐kong‐flu‐began‐in‐red‐china.html (viewed Aug 2025).
- 5. Influenza: the Hong Kong virus. Med J Aust 1968; 2: 962.
- 6. Chang WK. National influenza experience in Hong Kong, 1968. Bull World Health Organ 1969; 41: 349‐351.
- 7. A revised system of nomenclature for influenza viruses. Bull World Health Organ 1971; 45: 119‐124.
- 8. Lane WR. Influenza: the Hong Kong virus. Med J Aust 1969; 2: 58.
- 9. Crisis looms in city flu epidemic. The Sydney Morning Herald 1968; 11 Aug.
- 10. Ferris AA. Influenza in Melbourne, Australia, 1969. Bull World Health Organ 1969; 41: 399.
- 11. Cameron AS, Roder DM, Esterman AJ, Moore BW. Mortality from influenza and allied infections in South Australia during 1968–1981. Med J Aust 1985; 142: 14‐17.
- 12. WA parliament adjourned. Canberra Times 1968; 9 Aug.
- 13. Viboud C, Grais RF, Lafont BAP, et al; Multinational Influenza Seasonal Morality Study Group. Multinational impact of the 1968 Hong Kong influenza pandemic: evidence for a smoldering pandemic. J Infect Dis 2005; 192: 233‐248.
- 14. Arnold PC. Severity of Hong Kong influenza. Med J Aust 1969; 1: 943.
- 15. Apthorp BD. Hong Kong influenza. Br Med J 1969; 1: 49.
- 16. Page from the Staff News Magazine that circulated among Commonwealth Serum Laboratories’ employees describing the events around “flu furore” of 1969. CDC Museum Digital Exhibits. https://cdcmuseum.org/items/show/1123 (viewed Oct 2024).
- 17. Nguyen‐Van‐Tam JS, Hampson AW. The epidemiology and clinical impact of pandemic influenza. Vaccine 2003; 21: 1762‐1768.
- 18. Warburton MF. Desoxycholate‐split influenza vaccines. Bull World Health Organ 1969; 41: 639‐641.
- 19. Jester BJ, Uyeki TM, Jernigan DB. Fifty years of influenza A(H3N2) following the pandemic of 1968. Am J Public Health 2020; 110: 669‐676.
- 20. Peckham R. Viral surveillance and the 1968 Hong Kong flu pandemic. J Glob Hist 2020; 15: 444‐458.
- 21. Delloye T. How a “filthy” Woodstock still went ahead during 1968 Hong Kong flu pandemic that killed 100 000 Americans and infected everyone from President Lyndon Johnson to the Apollo 8 crew — and even Shamu the killer whale. The Daily Mail 2020; 19 May. https://www.dailymail.co.uk/news/article‐8320761/Woodstock‐occurred‐Hong‐Kong‐flu‐pandemic‐killed‐1‐million‐people‐worldwide‐100‐000‐Americans.html (viewed Oct 2024).
- 22. Warburton MF. Epidemiology of influenza in Australia and Papua New Guinea. Med J Aust 1973; 1 (SP1): 14‐18.
- 23. Willey K. Death toll unknown as flu epidemic worsens. The Sydney Morning Herald 1969; 25 Oct.
- 24. McIlraith S. Hong Kong flu cases point to epidemic. The Sydney Morning Herald 1969; 23 June.
- 25. Askin has flu. The Sydney Morning Herald 1970; 17 July.
- 26. Death of George Johnston. The Sydney Morning Herald 1970; 23 July.
- 27. Flu — send children home, teachers plead. The Sydney Morning Herald 1970; 29 July.
- 28. Flu delays funerals. The Sydney Morning Herald 1970; 23 July.
- 29. Cullimore H. Hell no we won’t go! Canberra: Australian War Memorial, 2020. https://www.awm.gov.au/articles/blog/blog/hell‐no‐we‐wont‐go (viewed June 2025).
- 30. Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol 2020; 7: 83‐101.
- 31. Australian Bureau of Statistics. Measuring Australia’s excess mortality during the COVID‐19 pandemic until August 2023 [website]. Canberra: ABS, 2023. https://www.abs.gov.au/articles/measuring‐australias‐excess‐mortality‐during‐covid‐19‐pandemic‐until‐august‐2023 (viewed Nov 2024).
- 32. Australian Bureau of Statistics. COVID‐19 mortality in Australia: deaths registered until 31 January 2024. Canberra: ABS, 2024. https://www.abs.gov.au/articles/covid‐19‐mortality‐australia‐deaths‐registered‐until‐31‐january‐2024 (viewed Dec 2024).
- 33. United States Centers for Disease Control and Prevention. Excess deaths associated with COVID‐19: provisional death counts for COVID‐19. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm (viewed Nov 2024).
- 34. Willebrand KS, Pischel L, Malik AA, et al. A review of COVID‐19 transmission dynamics and clinical outcomes on cruise ships worldwide, January to October 2020. Euro Surveill 2022; 27: 2002113.






We thank Peter C Arnold for the opportunity to discuss his recollections of the Hong Kong influenza pandemic.
No relevant disclosures.
Author contributions:
Matthew Brown: Conceptualization, writing – original draft, investigation, project administration, review and editing. Alan Hampson: Investigation, review and editing. John Gerrard: Conceptualization, investigation, supervision, review and editing.