The known: The incidence of silicosis in young workers in Australia is rising. Improving knowledge of how silicosis can be prevented and managed is urgently needed for research, funding, and policy decisions.
The new: Both people at risk of silicosis and those involved in their care or silicosis research regard eliminating exposure to silica, early diagnosis and better treatments, and reducing the personal and social impact of silicosis as priorities.
The implications: We have identified the research priorities of people directly affected by silicosis or involved in its prevention and management in Australia. They should guide future research, funding, and policy decisions.
Silicosis is a debilitating and potentially fatal parenchymal lung disease caused by the inhalation of respirable crystalline silica dust. There are no effective treatments,1,2 and people with silicosis experience reduced quality of life, reduced exercise tolerance, chest pain, impaired mental health, inability to work, and financial stress, and it also has an impact on their families and caregivers.3,4 Exposure to silica dust at work can also lead to chronic obstructive pulmonary disease,5,6,7,8 autoimmune conditions,9,10,11,12,13 an increased risk of lung cancer,14 and respiratory infections.15
The incidence of silicosis has markedly increased in Australia over the past decade, and is particularly associated with the processing of engineered stone products in the stone benchtop industry.4,16 The incidence of acute and accelerated silicosis (development of disease during a relatively short exposure interval) has also increased.16 Despite the ban on engineered stone in Australia since July 2024,17 many previously exposed benchtop workers are still at risk of developing silicosis, as are workers in other industries, such as construction, mining, quarrying, manufacturing, and tunnelling.18
There is an urgent need to improve the prevention and management of silicosis. Following the recommendations of the National Dust Disease Taskforce in 2021,4 the Australian government has recognised the importance of enhancing silicosis research. Research priorities must be defined and synthesised to facilitate a coordinated and strategic approach to reducing the impact of silicosis. The prevention and management of occupational lung disease requires collaboration by a wide variety of people in health care, workplace health and safety, industry, trade unions, and governments. In addition, research should be guided by the priorities and needs of the people living with or at risk of the disease and of their partners, caregivers, and families. As it is unclear what matters most to people affected by silicosis, the Australian government commissioned the Lung Foundation Australia to undertake a research priority setting project using the James Lind Alliance framework, which aims to develop a research agenda that is of direct relevance to those affected by a problem and will deliver meaningful outcomes.19 This approach has been used to establish research priorities for pulmonary fibrosis,20 chronic obstructive pulmonary disease,21 mesothelioma,22 and asthma.23
The aim of our study was to define research priorities in four areas — prevention, screening and diagnosis, treatment, and living with and managing the impacts of silicosis — according to the priorities of people living with silicosis, their partners and caregivers, workers at risk of silicosis, and health professionals and researchers.
Methods
We undertook a research priority setting exercise, based on the James Lind Alliance framework for research priority setting partnerships,19 during 14 April – 19 December 2023. We report our study according to the REPRISE guidelines24 (Supporting Information).
Participants
Two broad groups of people were eligible for participation in the exercise:
- workers at risk of silicosis because they had previously been or were currently exposed to silica dust; people with self‐reported diagnoses of silicosis or silica‐associated conditions; and partners or caregivers involved in the care of a person with silicosis; and
- health care providers, including respiratory and occupational medicine clinicians, nurses, allied health professionals; researchers involved in silicosis research, including exposure science, toxicology, occupational epidemiology, public health, implementation science, basic science, clinical science; and occupational health and safety professionals, including occupational hygienists, regulators, compensators, and union, industry, and legal representatives.
Study design
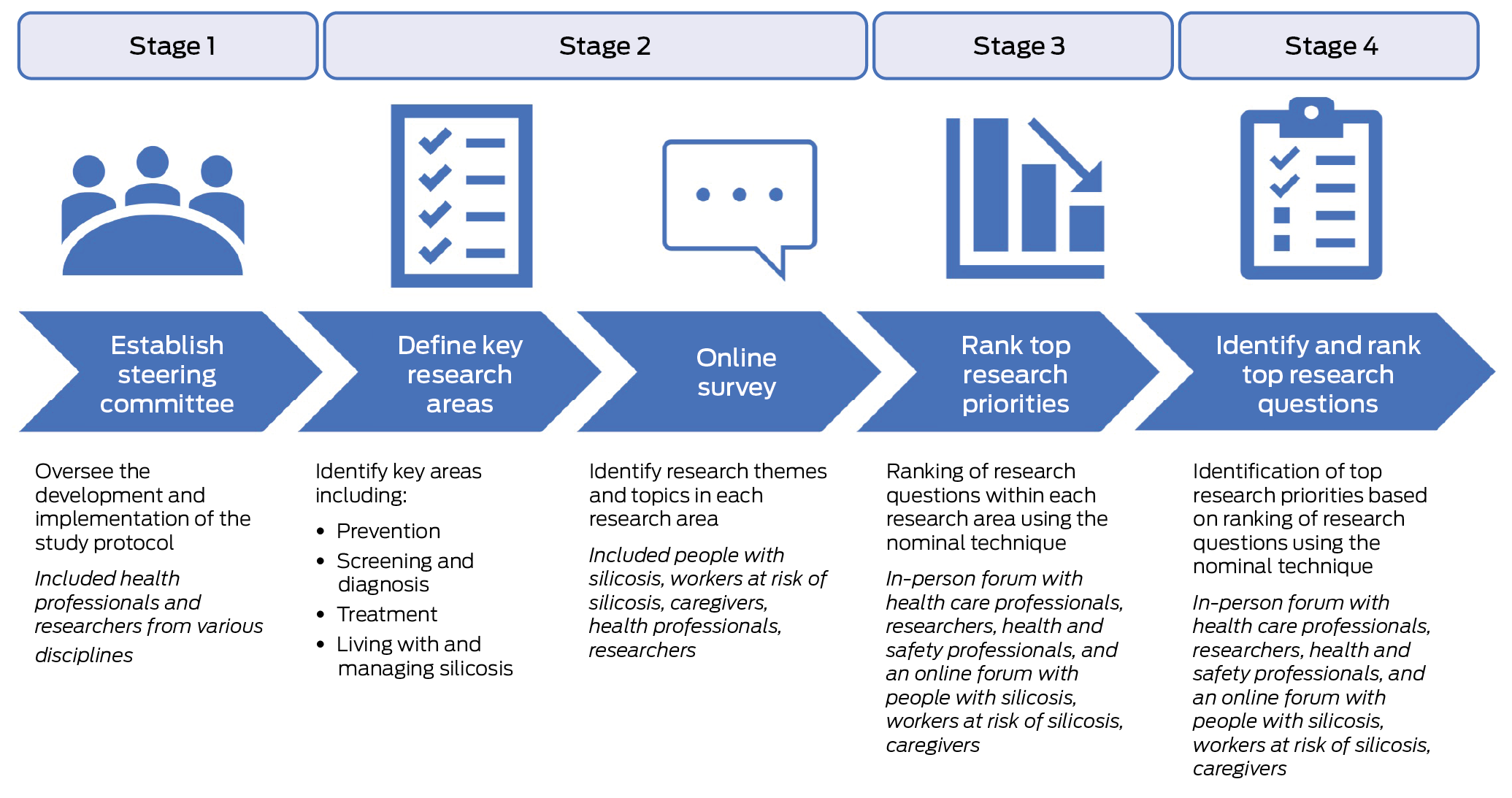
The research priority setting exercise comprised four stages: establishing the occupational lung disease network steering committee; identifying research topics in four research areas (prevention, screening and diagnosis, treatment, living and managing the impact of silicosis); reaching consensus about the top research topics in each research area to define research priorities; and synthesising research questions and ranking top research questions in each research area (Box 1).
We modified the James Lind Alliance approach to ensure coverage of broad research areas by focusing on research priorities, rather than selecting the top ten research questions. The aim of this choice was to encourage future support for a wide range of research into the primary, secondary, and tertiary prevention of silicosis.
Stage 1. Establishing the occupational lung disease network steering committee
Interested health professionals and researchers with expertise in the prevention, diagnosis, or treatment of silicosis were invited by Lung Foundation Australia to participate in the committee (Supporting Information, table 1). The Occupational Lung Disease Network steering committee, established on 14 April 2023, included seventeen people from a wide variety of disciplines (respiratory medicine, occupational and environmental health, radiology, genetics, basic science, qualitative research). The steering committee oversaw the development, refinement, and implementation of the project protocol.
Stage 2. Identifying research topics in four pre‐determined research areas
All participants were invited to complete an online survey, after providing active consent. They were recruited via Lung Foundation Australia professional and other mailing lists, study information flyers in occupational lung disease clinics, social media posts, and promotional material sent by email to key organisations and peak bodies. The online survey (Qualtrics; open for seven weeks: 1 July – 15 September 2023) included the open‐ended question: “What are the most important issues or topics you believe researchers should be working [on?]” in each of the four research areas: preventing silica dust exposure, screening or diagnosis of silicosis, treatment of silicosis, and living with silicosis (Supporting Information, table 2). Responses were coded as research themes by three post‐doctoral researchers (authors GT, SM, HB) with experience in qualitative and quantitative research methods.
Stages 3 and 4. Defining research priorities by consensus; synthesis and ranking of top research questions
Two research forums were held to present, prioritise, and discuss research topics and specific research questions, based on the survey responses in stage 2. Participants were recruited to attend the forums by advertisements in the online survey and through professional and public interest networks, such as Lung Foundation Australia (https://lungfoundation.com.au). Consent was implied by attendance at the forums.
Health care professionals, researchers, and occupational health and safety professionals were invited to participate in an in‐person forum, which involved small group discussions, each led by a member of the steering committee; the overall process was guided by an independent facilitator experienced in consumer‐based priority setting. Participants were provided with a summary of the online survey results prior to the forum. Each small group discussed these results and then ranked the five most important research priorities in each research area (using Slido, https://www.slido.com); the voting results were then presented to the entire group for discussion and feedback. A second round of small group discussions developed specific research questions for the top three to five priorities in each of the four areas, and then ranked the top three research questions. The results from each group were then reported to the entire group, and the results were analysed using a modified anonymous nominal technique25 (using Slido).
Workers at risk of silicosis, people with silicosis, and partners or caregivers were invited to participate in an online forum (Zoom), facilitated by the same independent facilitator and recorded for further analysis. Participants were presented with the research priorities generated at the in‐person forum, which they discussed in groups. Participants were then asked to rank the priorities (using Slido), and then discussed their relevance and importance.
Ethics approval
The project was approved by the Monash University Human Research Ethics Committee (project 39219).
Results
A total of 164 respondents completed the online survey (stage 2), of whom 105 were medical or research professionals, 34 were workers currently or formerly at risk of silicosis, eleven had confirmed silicosis, and fourteen were partners or caregivers (Supporting Information, table 3). A total of 47 topics were extracted from the completed questionnaires: fourteen topics in prevention, ten in screening and diagnosis, fifteen in treatment, and eight in living with and managing silicosis (Supporting Information, table 4). In stage 3, research questions were generated and ranked at the in‐person forum and were subsequently presented at the online forum; the online forum participants endorsed the research questions and did not suggest any additions or specific modifications (Box 2).
Demographic characteristics of forum participants
The in‐person forum (stage 3) was attended by 53 participants: eighteen academics (interest areas included occupational hygiene, pharmacology, epidemiology, basic science, allied health), sixteen health care professionals, six legal professionals, four regulators, three people from non‐governmental organisations, two occupational hygienists, two union representatives, and two industry representatives. The participants were purposively allocated to six small groups to achieve similar numbers of academics, health care professionals, legal professionals, and others in each group. The online forum was attended by thirteen people: eight with silicosis, one partner or caregiver, and five workers or community members at risk of silicosis. As the online survey was completed anonymously, it could not be determined whether forum participants had completed the survey. The top research priorities by participant group are shown in Box 3, Box 4, and Box 5; the top priorities for all forum participants are ranked in Box 6.
Preventing silica dust exposure and silicosis
Eliminating exposure was ranked by all participants as the highest research priority, but health care professionals noted that research in all components of the hierarchy of controls (elimination, substitution, isolation, engineering controls, personal protective equipment) were necessary for preventing silica dust exposure. Specific research questions included assessing the safety of new substituted materials and real‐time dust monitoring devices.
Identifying barriers to and enablers of effective compliance with the hierarchy of controls (for identifying and ranking safeguards for protecting workers from hazards, including elimination, substitution, engineering controls, administrative controls, personal protective equipment) was identified as an important research priority. Overcoming barriers specific to rural areas and for people from culturally and linguistically diverse backgrounds was also discussed.
Health care professionals acknowledged that research in implementation science (adopting what is known into policy and practice) is essential, including into increasing responsibility and accountability at all levels (government, employers, regulators, workers); active worker participation is central to averting silica‐related diseases. Similarly, the online forum participants reported that active participation by workers in qualitative patient‐centred research empowers them to speak up about health and safety matters, and that widespread cultural change was needed to reduce the stigma attached to speaking up in the workplace. Health care professionals ranked investigation of the best methods and the implementation of hierarchy of controls as a higher research priority than did workers and community members, who ranked education and overcoming barriers and changing workplace culture as priority research areas.
Screening and diagnosis
Early diagnosis was a high priority research area for all participant groups. They regarded national consistency in screening programs and diagnostic practices as important and saw potential benefits in a best model of screening practice for all workers formerly or currently exposed to silica dust. It was agreed that research into screening methods and screening intervals was required, and that any screening models should undergo a cost‐effectiveness analysis that compared the cost of screening with the numbers of lives, disability‐adjusted life‐years, and quality‐adjusted life‐years saved.
All participant groups also discussed the invasiveness of current screening methods and whether future research could develop less invasive alternatives. They also highlighted the benefit of a central registry or repository with minimum data standards that could benefit both researchers and workers, who noted that information can be lost when moving house or between workplaces. Workers and community members were somewhat reluctant to undergo screening because they feared receiving bad news (being diagnosed with silicosis), suggesting that any research into and implementation of a screening program and central registry should involve input by workers and community members.
Treatment of silicosis
People with silicosis described the “torture” of not being able to breathe and the importance of developing suitable treatment options for silicosis that are available in a timely and equitable manner across Australia. Health care professionals discussed the lack of effective treatments and how treatment innovation was required. Top research questions in this area included identifying biomarkers (including genetic markers) for screening, early diagnosis, estimating the risk of progression, and determining treatment; identifying relevant outcome measures of impairment and endpoints for treatment, including patient‐centred outcomes; and identifying the best experimental models of silicosis in humans, including models for testing therapies. Research priorities for worker and community member participants were reducing the symptom burden; that is the need for developing treatments that are directed at the pathogenesis of the disease, but also treatments that reduce symptom severity.
Living with and managing the impact of silicosis
Both health care professionals and workers and community members ranked research into maintaining mental health and wellbeing as the top priority in this area. Top research questions included identifying factors that influence mental health and how they can be modified, and developing an optimal multidisciplinary care model that is more strongly linked with the individual's care journey than with a medical model. Both groups also agreed that further research into the economic impact of disease is needed, both for the individual worker (including compensation) and on the government and societal levels. The development of a more holistic optimal care model based on evidence and the needs of the individual was a top priority.
Discussion
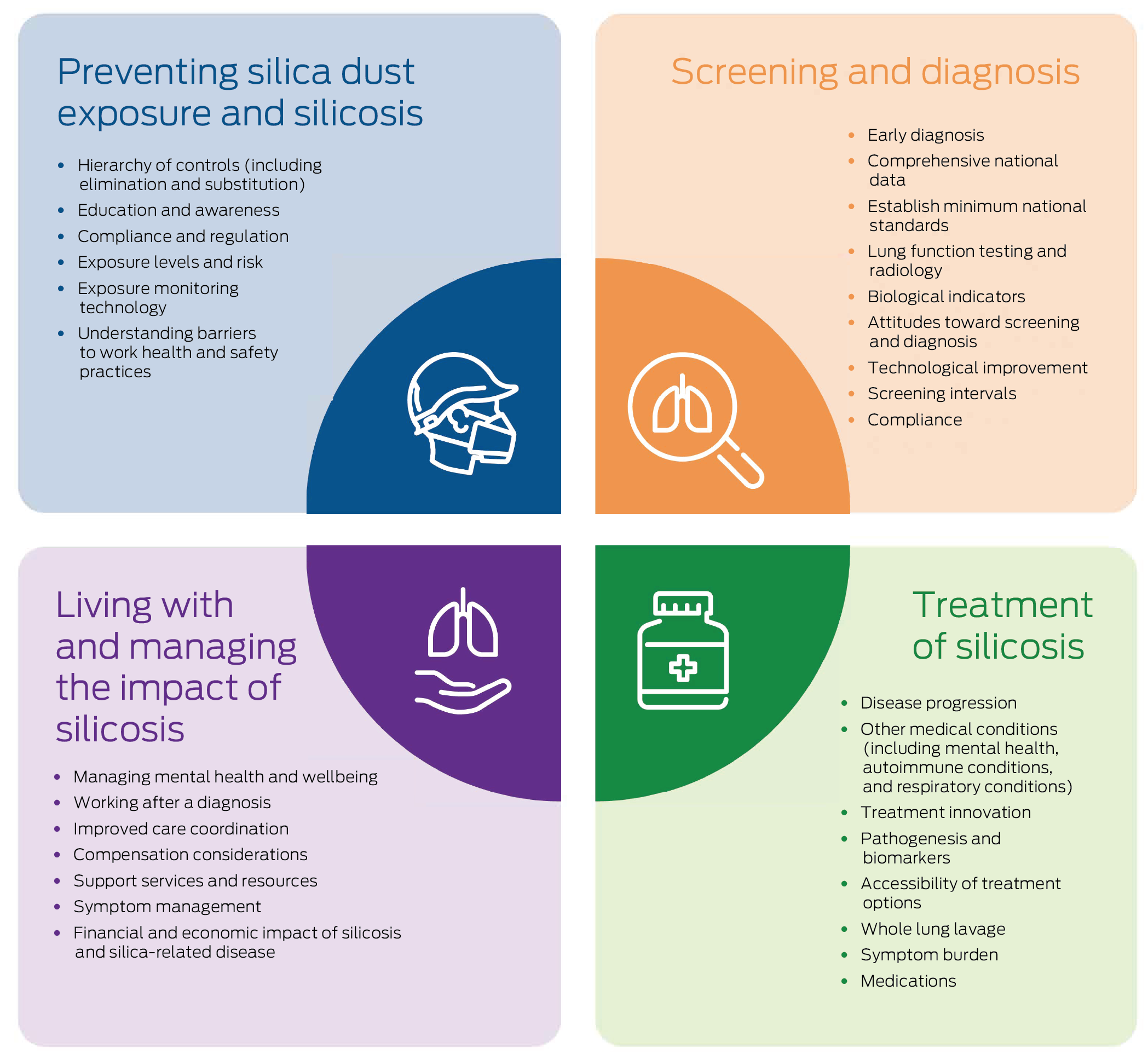
In our structured research priority setting exercise, we identified the top silicosis research priorities for health care professionals, researchers, and occupational health, safety professionals and for people with silicosis, at risk of silicosis, and partners or caregivers in four areas: preventing silica dust exposure and silicosis, screening and diagnosis, treatment, and living with and managing the impact of silicosis. Research into the hierarchy of controls, early diagnosis, treatments for preventing disease progression, and developing an optimal care model that includes mental health care were ranked as most important.
We used a structured approach for our research priority setting project, a modification of the James Lind Alliance method. We engaged with a wide variety of people professionally or personally concerned with silicosis to identify occupational disease research priorities. In each research area, the agreement between people with or at risk of silicosis and their caregivers and professionals from various disciplines about research priorities was reasonable. Both participant groups agreed that research into workplace controls and their implementation is important, as is improving education and awareness, compliance with preventive measures, and screening and diagnosis; they also agreed that earlier and nationally consistent screening and diagnosis practices were needed, and more knowledge about disease progression and the influence of other medical conditions, managing mental health, transitioning to new work, and improving care coordination.
However, some clear differences are important. The professional participants rated research into silicosis pathogenesis and biomarkers and technological considerations more highly than workers and their carers, who focused more on the barriers for and attitudes of workers, specific treatments, and managing symptoms as equally valuable for directing future research.
Our modified James Lind Alliance approach aimed to identify research priorities in four broad research areas to encourage future support for a broad scope of research into the primary, secondary, and tertiary prevention of silicosis, a rapidly evolving area. Our research setting project was conducted before the Australian government announced its ban on engineered stone products, and research priorities may change as policy changes. However, our deliberately broad and inclusive scope allows for evolution of both policy and knowledge regarding silicosis, and could inform research priorities in countries where engineered stone is still used. Even with the ban, many workers already exposed to engineered stone products will still require screening and diagnosis, and a proportion will unfortunately develop silicosis and require treatment and support with living with the disease. Substitution with materials not including silica needs to be investigated. Further, there are many other occupational sources of respirable crystalline silica, including in construction and mining, where research should be focused.
One component of the James Lind Alliance approach is uncertainty verification; that is, determining whether an uncertainty has already been investigated in earlier research. The James Lind Alliance suggests examining each question using high level evidence from systematic reviews, guidelines, and large scale registry databases.19 However, as silicosis research, particularly that related to engineered stone, is relatively recent, high level evidence is unlikely to be available. As part of our protocol, we plan to examine the impact of our research priority setting project in 2030, when the evidence base should be more substantial.
During the research priority setting project, we noted a distinction between the need for research to answer specific questions (for example: How can novel diagnostic and prognostic biomarkers of silica‐related disease be identified?) and research into how to best translate evidence into practice. Implementation research requires the involvement of not only researchers, but also of governments, policy makers, regulators, and workers, as was noted in the forums. It is hoped that the generation of research priorities will not only assist researchers, but also others involved in improving the health and safety of people working with silica and those with silicosis.
Limitations
Our study involved a wide variety of people in Australia with an interest in silicosis to identify research priorities, conducted with a systematic approach. The recruitment process for our online survey and forums precludes any conclusions about the representativeness of our participants. The online forum avoided the need for travel, enabling the participation of people with or at risk of silicosis in different locations. However, the inherent limitations of virtual discussions, compared with in‐person discussions, cannot be overlooked. The relatively small number of people at risk of or living with silicosis involved in the study, and none from culturally and linguistically diverse backgrounds, who comprise a substantial proportion of stone benchtop workers,16 were also limitations. Future research should actively involve workers and other community members in its design and implementation.
Conclusion
In a silicosis research priority exercise, we found that research into the elimination of exposure and other hierarchy of controls of silica use, early diagnosis, treatment for preventing disease progression, and the development of an optimal care model, including mental health care, were the top research priorities for people with either professional or personal interest in silicosis. Our findings could guide future silicosis research and policy development.
Box 2 – The top silicosis research questions determined by participants at two post‐survey forums, by research priority area
|
Research priority area |
Research priorities |
Research questions* |
|||||||||||||
|
|
|||||||||||||||
|
Preventing silica dust exposure and silicosis |
|
|
|||||||||||||
|
Screening and diagnosis |
|
|
|||||||||||||
|
Treatment |
|
|
|||||||||||||
|
Living with and managing the effects of silicosis |
|
|
|||||||||||||
|
|
|||||||||||||||
|
* A more comprehensive list of research questions is included in the Supporting Information, table 5. |
|||||||||||||||
Box 3 – Ranking of research priorities by research area: results of the in‐person forum for 53 health care professionals, researchers, and occupational health and safety professionals*
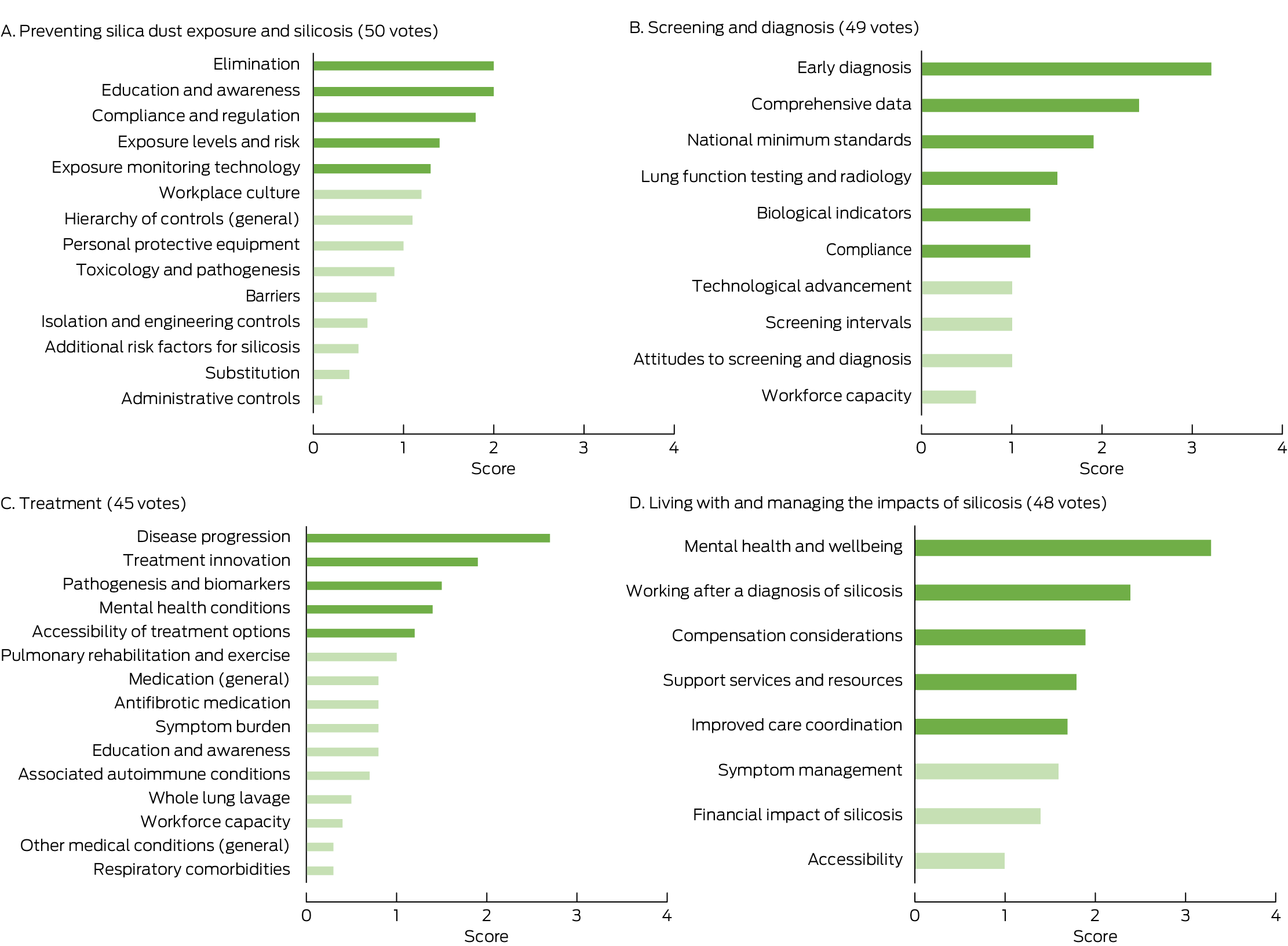
* For derivation of ranking poll scores, see reference 26.
Box 4 – Ranking of research priorities by research area: results of the online forum for thirteen people with silicosis, workers at risk of silicosis, and partners or caregivers*
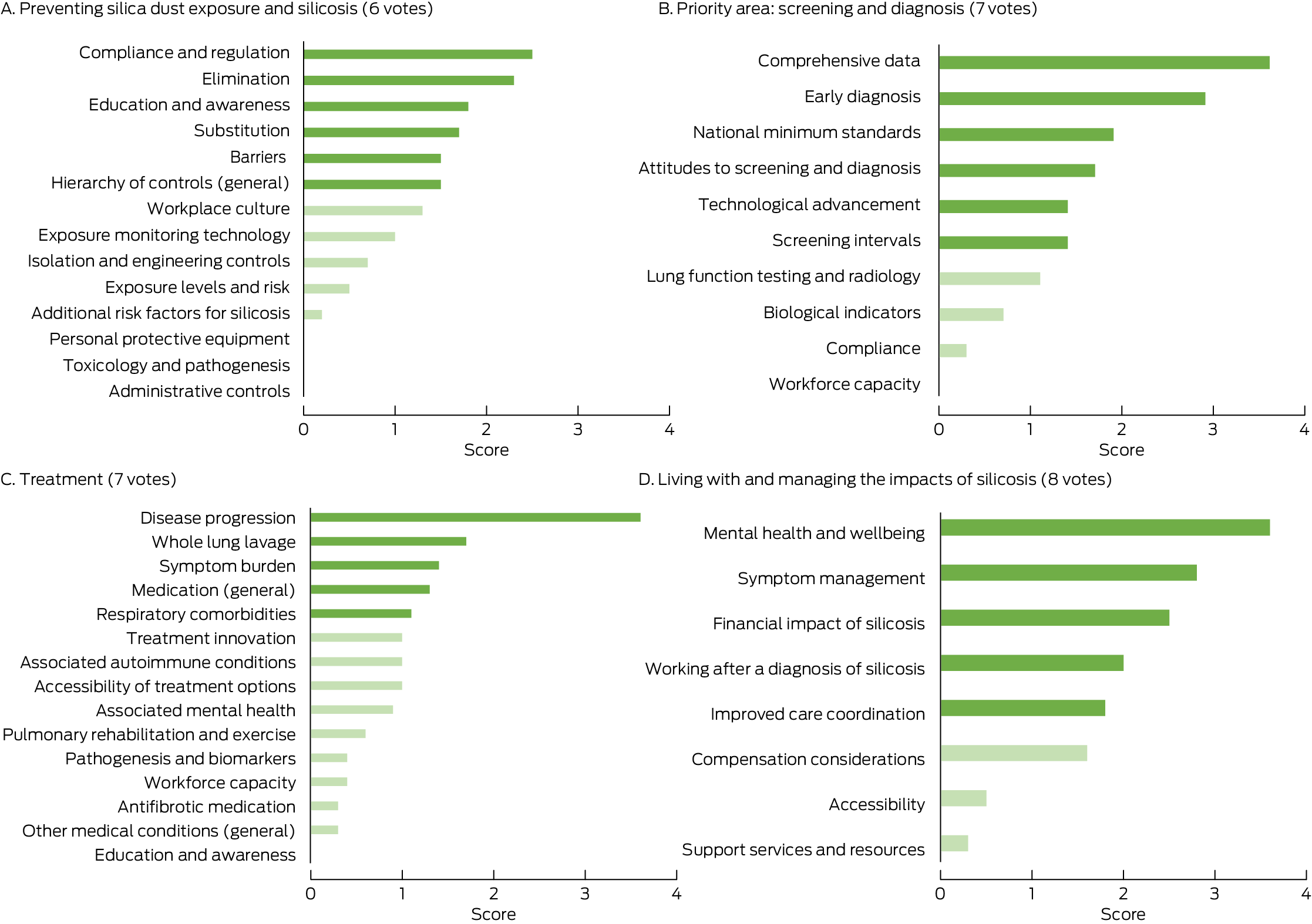
* For derivation of ranking poll scores, see reference 26.
Box 5 – Ranking of research priorities by research area: comparison of the two forum participant groups
|
Outcome |
Preventing silica exposure and silicosis |
Screening and diagnosis |
Treatment |
Living with silicosis |
|||||||||||
|
|
|||||||||||||||
|
Consensus priorities |
|
|
|
|
|||||||||||
|
Higher priority for health care professionals, researchers, and occupational health and safety professionals |
|
|
|
|
|||||||||||
|
Higher priority for people with silicosis, workers at risk of silicosis, and partners or caregivers |
|
|
|
|
|||||||||||
|
|
|||||||||||||||
|
|
|||||||||||||||
Received 13 May 2024, accepted 7 March 2025
- Hayley Barnes1,2,3
- Sharna Mathieu4,5
- Deborah C Glass1
- Malcolm R Sim2
- Lin Fritschi6
- Joanne L Dickinson7
- Daniel C Chambers8,9
- Tim R Driscoll10
- Graeme Edwards11,12
- Nikky LaBranche13
- Catherine Jones10
- Jane E Bourke14
- Ryan F Hoy1,3
- Christine R Jenkins10,15
- Simon Apte8,9
- Anne Holland2,3
- Gabriella Tikellis2
- 1 Monash Centre for Occupational and Environmental Health, Monash University, Melbourne, VIC
- 2 Monash University, Melbourne, VIC
- 3 Alfred Health, Melbourne, VIC
- 4 Lung Foundation Australia, Brisbane, QLD
- 5 Griffith University, Brisbane, QLD
- 6 Curtin University, Perth, WA
- 7 Menzies Research Institute Tasmania, University of Tasmania, Hobart, TAS
- 8 The University of Queensland, Brisbane, QLD
- 9 The Prince Charles Hospital, Brisbane, QLD
- 10 The University of Sydney, Sydney, NSW
- 11 Royal Australasian College of Physicians, Sydney, NSW
- 12 Work and Health Risk Management, Brisbane, QLD
- 13 Sustainable Minerals Institute, the University of Queensland, Brisbane, QLD
- 14 Biomedicine Discovery Institute, Monash University, Melbourne, VIC
- 15 The George Institute for Global Health, Sydney, NSW
Open access:
Open access publishing facilitated by Monash University, as part of the Wiley – Monash University agreement via the Council of Australian University Librarians.
Data Sharing:
The de‐identified data we analysed are not publicly available, but requests to the corresponding author for the data will be considered on a case‐by‐case basis.
This project was supported by the Australian government via the Lung Foundation Australia. The Australian government did not have any role in the planning, writing, or publication of this work. We thank Catherine Runge (Lung Foundation Australia), who provided support during the data analysis phase, and Allison Jaure (University of Sydney), who facilitated the sessions.
Anne Holland is the President of the Thoracic Society of Australia and New Zealand.
- 1. Barnes H, Goh NSL, Leong TL, Hoy R. Silica‐associated lung disease: an old‐world exposure in modern industries. Respirology 2019; 24: 1165‐1175.
- 2. Hoy RF, Jeebhay MF, Cavalin C, et al. Current global perspectives on silicosis: convergence of old and newly emergent hazards. Respirology 2022; 27: 387‐398.
- 3. Hoy RF, Chambers DC. Silica‐related diseases in the modern world. Allergy 2020; 75: 2805‐2817.
- 4. National Dust Disease Taskforce (Australian Department of Health). Final report to Minister for Health and Aged Care. Department of Health and Aged Care. June 2021. https://www.health.gov.au/sites/default/files/documents/2022/07/national‐dust‐disease‐taskforce‐final‐report.pdf (viewed Mar 2025).
- 5. Fan Y, Xu W, Wang Y, et al. Association of occupational dust exposure with combined chronic obstructive pulmonary disease and pneumoconiosis: a cross‐sectional study in China. BMJ Open 2020; 10: e038874.
- 6. Grahn K, Gustavsson P, Andersson T, et al. Occupational exposure to particles and increased risk of developing chronic obstructive pulmonary disease (COPD): a population‐based cohort study in Stockholm, Sweden. Environ Res 2021; 200: 111739.
- 7. Peng C, Yan Y, Li Z, et al. Chronic obstructive pulmonary disease caused by inhalation of dust: a meta‐analysis. Medicine (Baltimore) 2020; 99: e21908.
- 8. Murgia N, Gambelunghe A. Occupational COPD. The most under‐recognized occupational lung disease? Respirology 2022; 27: 399‐410.
- 9. Muntyanu A, Milan R, Rahme E, et al; Canadian Scleroderma Research Group. Exposure to silica and systemic sclerosis: a retrospective cohort study based on the Canadian Scleroderma Research Group. Front Med (Lausanne) 2022; 9: 984907.
- 10. McCormic ZD, Khuder SS, Aryal BK, et al. Occupational silica exposure as a risk factor for scleroderma: a meta‐analysis. Int Arch Occup Environ Health 2010; 83: 763‐769.
- 11. Patel S, Morrisroe K, Proudman S, et al; Australian Scleroderma Interest Group. Occupational silica exposure in an Australian systemic sclerosis cohort. Rheumatology (Oxford) 2020; 59: 3900‐3905.
- 12. Boudigaard SH, Schlünssen V, Vestergaard JM, et al. Occupational exposure to respirable crystalline silica and risk of autoimmune rheumatic diseases: a nationwide cohort study. Int J Epidemiol 2021; 50: 1213‐1226.
- 13. Mehri F, Jenabi E, Bashirian S, et al. The association between occupational exposure to silica and risk of developing rheumatoid arthritis: a meta‐analysis. Saf Health Work 2020; 11: 136‐142.
- 14. Guha N, Straif K, Benbrahim‐Tallaa L. The IARC Monographs on the carcinogenicity of crystalline silica. Med Lav 2011; 102: 310‐320.
- 15. Ehrlich R, Akugizibwe P, Siegfried N, Rees D. The association between silica exposure, silicosis and tuberculosis: a systematic review and meta‐analysis. BMC Public Health 2021; 21: 953.
- 16. Hoy RF, Dimitriadis C, Abramson M, et al. Prevalence and risk factors for silicosis among a large cohort of stone benchtop industry workers. Occup Environ Med 2023; 80: 439‐446.
- 17. Safe Work Australia. Decision regulation impact statement: Prohibition on the use of engineered stone. 27 Oct 2023. https://www.safeworkaustralia.gov.au/doc/decision‐regulation‐impact‐statement‐prohibition‐use‐engineered‐stone (viewed Mar 2025).
- 18. Carey R, Fritschi L. The future burden of lung cancer and silicosis from occupational silica exposure in Australia: a preliminary analysis. Report commissioned by the Australian Council of Trade Unions (ACTU). Apr 2022. https://www.curtin.edu.au/about/wp‐content/uploads/sites/5/2022/07/FEFreport_formatted.pdf (viewed Mar 2025).
- 19. James Lind Alliance. The James Lind Alliance guidebook; version 10. Mar 2021. https://www.jla.nihr.ac.uk/jla‐guidebook (viewed Mar 2025).
- 20. Tikellis G, Tong A, Lee JYT, et al. Top 10 research priorities for people living with pulmonary fibrosis, their caregivers, healthcare professionals and researchers. Thorax 2021; 76: 575‐581.
- 21. Alqahtani JS, Aquilina J, Bafadhel M, et al. Research priorities for exacerbations of COPD. Lancet Respir Med 2021; 9: 824‐826.
- 22. Stephens RJ, Whiting C, Cowan K; James Lind Alliance Mesothelioma Priority Setting Partnership Steering Committee. Research priorities in mesothelioma: a James Lind Alliance Priority Setting Partnership. Lung Cancer 2015; 89: 175‐180.
- 23. Majellano EC, Bell RL, Flynn AW, et al. Identifying the asthma research priorities of people with asthma, their carers and other stakeholders. Respirology 2023; 28: 636‐648.
- 24. Tong A, Synnot A, Crowe S, et al. Reporting guideline for priority setting of health research (REPRISE). BMC Med Res Methodol 2019; 19: 243.
- 25. McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm 2016; 38: 655‐662.
- 26. Slido team. How we calculate the scores [help centre post]. https://community.slido.com/live‐polls‐quizzes‐and‐surveys‐55/create‐and‐run‐a‐ranking‐poll‐727#:~:text=in%20Present%20mode‐,How%20we%20calculate%20the%20scores (viewed July 2025).






Abstract
Objectives: To identify the silicosis research priorities of people living with silicosis, workers at risk of silicosis, their partners and caregivers, and of health professionals and researchers.
Study design: Research priority setting exercise; modified James Lind Alliance framework for research priority setting partnerships, comprising an online survey followed by two forums in which thematic analysis and nominal group analysis were used to establish a list of research priorities.
Setting, participants: People with or at risk of silicosis, their partners or caregivers (survey, online forum) and health care professionals, researchers, health and safety professionals (survey, in‐person forum), recruited 14 April – 19 December 2023.
Main outcome measures: Research priorities in four pre‐identified areas: prevention, screening and diagnosis, treatment, and living with and managing the impact of silicosis.
Results: A total of 164 survey respondents (105 medical or research professionals, 34 workers currently or formerly at risk of silicosis, eleven people with confirmed silicosis, and fourteen partners or caregivers) identified 47 key research topics. Fifty‐three health care professionals and thirteen people with or at risk of silicosis and their caregivers then ranked the research topics and developed research questions at the two forums. The highest ranked research priorities were research into assessment and optimisation of the hierarchy of controls, compliance and regulation, establishing minimum standards and developing innovative screening methods, early diagnosis, development of effective treatments, identification of biomarkers for risk of progression, developing an optimal care model that includes mental health care, and estimating the economic impact of silicosis. Both participant groups agreed that research into workplace controls is important, as is improving education and awareness, compliance with preventive measures, and screening and diagnosis, including nationally consistent screening and diagnosis practices. The professional participants rated research into silicosis pathogenesis and biomarkers and technological considerations higher than workers and their carers, who focused more on the barriers for and attitudes of workers, specific treatments, and managing symptoms.
Conclusions: Research into eliminating exposure to silica, early diagnosis of silicosis, preventing disease progression, and reducing the impact of disease were the top research priorities for people with professional or personal interests in silicosis. Our findings should guide research directions and inform policy development.