The known: Tailored strength and balance exercises help maintain mobility and reduce falls in older people receiving aged care. However, access to physiotherapists for these programs is limited in Australian aged care.
The new: The TOP‐UP intervention, a co‐designed telephysiotherapy program that combined virtual assessments, tailored exercise videos, and aged care worker support, improved the mobility, reduced the fall risk and pain, and enhanced the quality of life of older people receiving community or residential aged care.
The implications: Locally supported telephysiotherapy exercise programs can improve health and quality of life of people receiving aged care. It is a feasible and expandable solution when in‐person physiotherapy is impractical.
Older people receiving aged care often have multiple health problems, including dependence on others for basic needs and restricted mobility.1 In the United States, mobility disability affects 35% of people aged 70 years or older. The World Health Organization recommends that all adults undertake 150–300 minutes of moderate intensity activity per week, including balance and strength training, to improve mobility.2 The 2018 Australian Sunbeam trial found that a six‐month physiotherapist‐led moderate intensity strength and balance exercise program improved mobility and reduced falls among people in aged care.3 However, an updated Cochrane literature review found that falls prevention in residential aged care requires ongoing, tailored strength and balance exercise delivered at moderate intensity for at least one hour each week.4,5
The Australian Royal Commission into Aged Care highlighted the need for interventions that improve mobility and reduce falls in aged care.6,7 Physiotherapists have the expertise to deliver tailored exercise programs.3 Despite the limited resources of allied health services such as physiotherapy,8 recent residential aged care funding reforms provide an opportunity for optimising use of staff time, enhancing care quality, and introducing innovative solutions, such as telehealth, particularly in regional areas.9
Telehealth uses information and communication technology to deliver health care services remotely.10 The coronavirus disease 2019 (COVID‐19) pandemic accelerated infrastructure development and the adoption of telehealth by older people and health care professionals, making it a viable option in aged care.11 However, evidence supporting the value of telehealth for delivering physiotherapy (telephysiotherapy) is limited. Our recent systematic review found that few randomised controlled trials had specifically evaluated the effect of telephysiotherapy on outcomes such as mobility, falls, and quality of life for people in aged care.12
We therefore assessed the implementation of the Telephysiotherapy for Older People (TOP‐UP) program and its effectiveness for improving mobility (sit‐to‐stand performance, balance, gait speed), physical function (fall rate, fall risk, pain, physical activity), mobility goal attainment, and quality of life among adults aged 65 years or older who were receiving at‐home or residential aged care. We also examined implementation outcomes (adoption, reach, fidelity, and dose delivered) to provide information that could inform health care policy, clinical practice, and the design of telephysiotherapy services as part of aged care.
Methods
The TOP‐UP trial was a two‐arm, pragmatic, hybrid type 1 effectiveness–implementation randomised controlled trial, conducted from 1 September 2021 to 30 November 2023.13 Trial and protocol reporting were guided by the CONsolidated Standards Of Reporting Trials (CONSORT) statement,14 the Template for Intervention Description and Replication (TIDieR) checklist,15 and the Consensus on Exercise Reporting (CERT) guidelines.16 The trial was registered prospectively with the Australian New Zealand Clinical Trials Registry (ACTRN12621000734864; 10 June 2021).
Participants
The TOP‐UP trial was conducted in collaboration with aged care providers who offer home or residential aged care services in metropolitan, regional, and remote areas of New South Wales, Victoria, and Western Australia. Aged care providers were recruited through research networks and direct outreach, including calling a broad range of providers in different regions to ensure geographic and service diversity. Providers assisted with participant recruitment, using a standardised screening form. The eligibility criteria for participants were the willingness to use a tablet computer for video consultations and to commit to two hours of weekly exercise, and adequate sensory, neurological, cognitive, and English language skills for participation. Exclusion criteria were severe cognitive impairment (Modified Telephone Interview for Cognitive Status score of 10 or less17), inability to walk ten metres, current participation in a physiotherapist‐led exercise program, and life expectancy less than six months. All participants provided written consent, together with an enduring power of attorney if required by aged care service management. Participant agency was a priority, and we ensured that the study was clearly explained and that the willingness to participate was confirmed before consent was requested.
Randomisation and blinding
Baseline data were collected during a Zoom meeting prior to randomisation by research team physiotherapists, with the support of aged care workers. Participants were randomly assigned to the TOP‐UP program or to the waiting list control group using a centralised web system with random permutation blocks of two and four, stratified by aged care type. A statistician computer‐generated the allocation sequence, independent of recruitment; enrolment staff did not have access to the sequence. The nature of the intervention precluded blinding of participants or care providers to allocation; outcomes assessors and data analysts were blinded through role separation and participant instructions. Cognitive impairment was assessed with the Modified Telephone Interview for Cognitive Status (range, 0–41; severe: score of 10 or less; moderate: 11–20; mild: 21–30; no impairment: 31–4017). Readiness to adopt new technology was assessed with the Technology Readiness Index (low scores = low readiness because of perceived complexity or lack of usefulness).18
The TOP‐UP intervention
Experienced aged care physiotherapists, employed or contracted by our aged care partners and independent of the research team members who conducted follow‐up assessments, delivered ten Zoom sessions over six months, during weeks 1, 3, 5, 7, 9, 12, 16, 20, 22, and 24 of the trial. The sessions described tailored balance and strength exercises in the Otago Exercise Program.19 Participants were encouraged to independently undertake moderate intensity exercise (Borg scale, 12–14 of 20)20 for two hours each week. Participants had access to further information in the TOP‐UP website and booklet (https://www.topupexercise.com.au); aged care support workers assisted with telephysiotherapy appointments and supervised weekly 30‐miunte exercise sessions. Physiotherapists prescribed exercise selections for independent and supervised sessions of gradually increasing intensity, for safety reasons. To maximise adherence, physiotherapists and support workers received one hour of training (via Zoom) in health coaching and behaviour change strategies from the research team.21,22 Adherence to the program was tracked in participant self‐report diaries.
Control group
Participants in the control group received usual care, including seated exercise, non‐strength/balance exercise programs, and massage and heat therapies. They were offered a three‐month TOP‐UP program after completion of the study.
Outcomes
All outcomes were assessed at baseline and six months after randomisation. The primary outcome was mobility as indicated by the combined score from the 12‐point Short Physical Performance Battery (SPPB), which assesses standing balance, gait, and timed sit‐to‐stand. The SPPB score is a predictor of mortality, care admission, and disability.23
The secondary outcomes were:
- fall rate (falls per person) and falls risk (proportion of people who experienced at least one fall), based on incident reports (residential care) or self‐report diaries (home care);
- SPPB components (five times sit‐to‐stand, four‐step balance, gait speed);
- pain, assessed with a visual analogue scale (1–10 scale);24
- mobility goal attainment, assessed with the 5‐point Goal Attainment Scale (+2 = much better than expected, +1 = somewhat better than expected, 0 = expected level, –1 = somewhat less, –2 = much less);25
- physical activity, assessed with the Incidental and Planned Exercise Questionnaire (IPEQ);26 and
- quality of life, assessed with four measures: the EuroQol 5‐dimension 5‐level (EQ‐5D‐5L) visual analogue scale (range, 0–100);27 the question “Compared to six months ago, how would you rate your quality of life?” (–2 = much worse, 0 = no change, +2 = much better); reported balance self‐confidence (1 = excellent to 5 = poor); and reported fear of falling (1 = not at all to 5 = extremely).28
Implementation outcomes were assessed to inform future program design, delivery modifications, and expansion:29
- adoption: proportion of invited aged care services that participated in the trial;
- reach: proportion of aged care service users who were screened, consented to participation, and participated in the intervention;
- fidelity: the number and duration of physiotherapy and support worker‐assisted sessions completed by participants; and
- dose delivered: total amount of exercise undertaken by participants.
To evaluate the generalisability of the intervention, feasibility factors, such as the proportion and representativeness of people still participating at six months, were considered throughout the study.
We also examined program acceptability, barriers, facilitators, and uptake factors in surveys and interviews with participants, physiotherapists, support workers, and service managers. Our thematic analysis of interview data has been reported elsewhere;30 in this article, we discuss only the trial participant survey responses. All adverse events, including falls, injuries, and deaths, were documented in incident reports (residential care) or participant diaries (home care). Two investigators independently reviewed each event, using medical records and care documentation to assess whether it was related to the intervention and its impact on study viability. We established a data monitoring committee to review serious unexpected events related to the intervention.
Sample size
We determined that 240 participants (120 per group) were required to provide 80% statistical power to detect a 0.9‐point between‐group difference in 12‐point SPPB scores at six months, assuming a standard deviation (SD) of 2.8, α = 0.05, and 20% attrition. We defined a 0.5‐point between‐group difference in SPPB as being clinically significant.31 This sample size was also expected to be adequate for detecting 10–15% between‐group differences in the secondary outcomes.
Statistical analysis
We registered our statistical analysis plan with the Open Science Framework prior to data analysis (https://osf.io/qyt5a; 29 April 2024). We used a modified intention‐to‐treat approach; we analysed data for all participants for whom follow‐up data were available as part of their original randomised group, regardless of intervention adherence. Participants lost to follow‐up were excluded from outcomes analyses; missing data were not imputed. The statistical significance of between‐group differences in mobility (SPPB scores) and other continuous outcomes at six months was assessed in linear regression models adjusted for baseline scores; we report adjusted mean differences with 95% confidence intervals (CIs). The statistical significance of between‐group differences in ordinal outcomes (including SPPB components, Goal Attainment Scale scores, quality of life) was assessed in ordinal regression models adjusted for baseline; we report adjusted odds ratios (aORs) with 95% CIs. The statistical significance of the difference in fall rate was assessed using negative binomial regression (with follow‐up time as offset), adjusted for baseline; we report the adjusted incidence rate ratio (IRR) with 95% CI. We report fall risk, analysed using log‐binomial regression, as estimate relative risk (RR) with 95% CI. Other dichotomous outcomes (pain improvement, mobility goal met, self‐reported improvement in quality of life) were analysed using logistic regression; we report adjusted odds ratios (aORs) with 95% CIs. We also undertook pre‐specified subgroup analyses by gender, care type (home care, residential aged care), and cognitive impairment status that included interaction terms. No post hoc analyses were performed, and no interim analyses planned. Stopping guidelines were developed prior to trial commencement. Implementation outcomes are summarised numerically and descriptively.
Ethics approval
The human research ethics committee of the Sydney Local Health District (Concord) approved the trial (CH62/6/2021‐009).
Results
During 1 September 2020 – 31 March 2023, 1348 people aged 65 years or older were screened at 27 sites, of whom 242 people were recruited for the trial: 120 were randomised to the intervention group (residential aged care, 51; home care, 69), 122 to the control group (residential aged care, 52; home care, 70) (Box 1). The mean age of the 242 participants was 83 years (standard deviation [SD], 8 years; range, 65–100 years). Cognitive impairment was detected in 108 participants (45%; mild impairment in 76 and moderate impairment in 32 people). Fifty‐one participants (21%) had prior telehealth experience; the mean Technology Readiness Index score was 2.1 (SD, 0.8; range, 1.0–4.6). The baseline demographic characteristics of the two groups were similar (Box 2).
A total of 192 participants (79%) completed the six‐month mobility assessment (primary outcome). The mean age at baseline of the 50 people who withdrew from the study was similar to that for the 192 available for the six‐month follow‐up (82 [SD, 9] v 82 [SD, 8] years), as was the baseline mobility score (5.1 [SD, 2.9] v 5.5 [SD, 2.9]), and the proportion of women (33 of 50, 66% v 127 of 192, 66%). The mean pain visual analogue score was higher for the participants who withdrew (4.6 [SD, 2.9] v 3.9 [SD, 3.0]) and the proportion with cognitive impairment was larger (26 of 50, 52% v 82 of 192, 43%).
One minor adverse event was related to the intervention, a non‐injuring fall, but there were no serious adverse events. The most frequent reasons for withdrawing from the trial were poor health, including COVID‐19 (22 participants, 9%) and deaths unrelated to the intervention (sixteen participants, 7%: cerebrovascular disease, six; chronic heart disease, five; cancer, one; cause unknown, four people). As no concerns were reported by staffs at the trial sites, these deaths were deemed unrelated to the intervention, consistent with our safety monitoring procedures.
Primary outcome
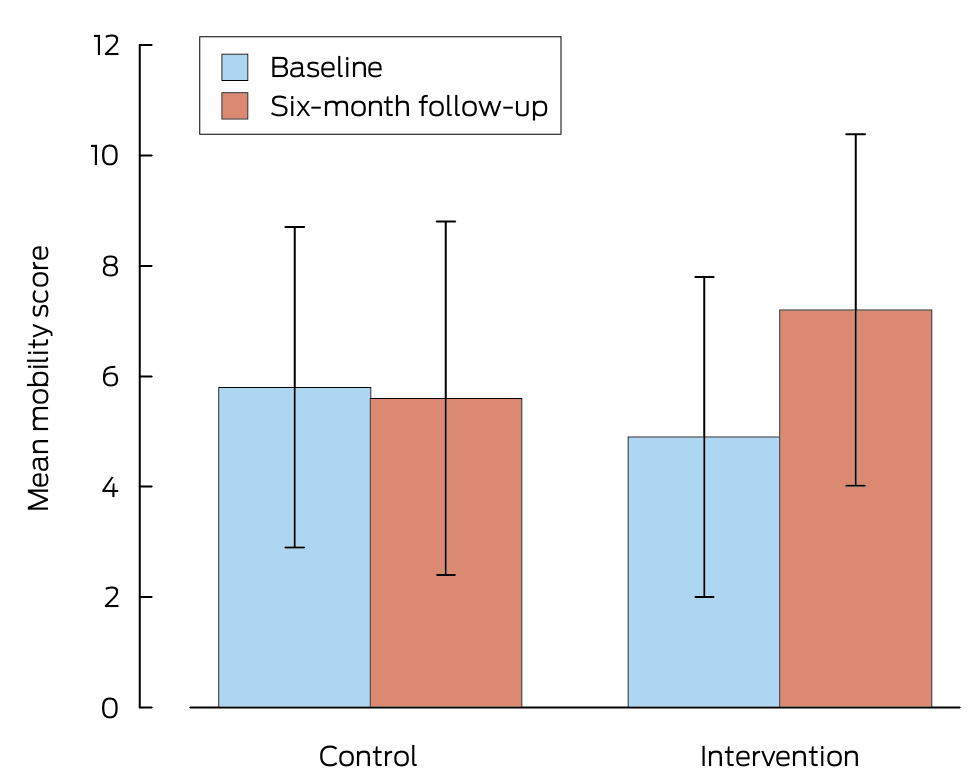
After adjusting for baseline mobility scores, the mean difference in mobility score at six months (intervention v control group) was 2.1 (95% confidence interval [CI], 1.4–2.7) points (Box 3, Box 4); the estimated mean difference was similar after also adjusting for study site (2.0 points; 95% CI, 1.4–2.7 points).
Secondary outcomes
Sit‐to‐stand performance was more likely to improve in intervention participants than in control participants (aOR, 2.7; 95% CI, 1.3–4.3); in comparison with the control group, they needed less hand support to stand up, their gait was more rapid over 2.4 m (adjusted mean difference, 0.9 [95% CI, –1.6 to –0.1] seconds), and they were more likely to meet their mobility goals (aOR, 14.1; 95% CI, 4.1–48.5). Pain visual analogue scores (adjusted mean difference, –1.1 points; 95% CI, –1.8 to –0.3 points) and planned exercise participation (adjusted mean difference, 1.7 [95% CI, 1.1–2.3] hours/week) were better for the intervention than the control group (Box 3). Intervention group outcomes were also better than for the control group with respect to the sit‐to‐stand, balance, and gait speed SPPB components (raw data: Supporting Information, table 1).
Mobility goals were met or exceeded by 48 of 92 intervention group participants (53%) and seven of 100 control group participants (7%) (Supporting Information, table 2). At six months, intervention participants reported greater quality of life (EQ‐5D‐5L visual analogue scale: adjusted mean difference, 6.2; 95% CI, 1.8–10.7); they were more likely to report improved quality of life (aOR, 7.0; 95% CI, 3.4–14.2), and 47 intervention group participants (51%) reported that their quality of life had improved between baseline and follow‐up, compared with thirteen control participants (13%) (Box 5). Intervention group participants also reported greater self‐confidence about balance (adjusted mean difference, –0.3 [95% CI, –0.2 to –0.5] points) and of falling (adjusted mean difference, –0.5 [95% CI, –0.3 to –0.5] points).
Over six months, 58 falls were recorded in the intervention group and 96 for the control group, but the difference in incidence was not statistically significant (incidence rate ratio, 0.60; 95% CI, 0.35–1.01) (Box 6). By six months, six of 92 participants in the intervention group (10%) had experienced two or more falls, and 19 of 100 participants in the control group (19%). The mean surveillance period was slightly longer in the intervention group (196 [SD, 37] days) than in the control group (180 [SD, 17] days). The mean number of falls per participant over six months was 0.52 (SD, 1.45) per person in the intervention group and 0.96 (SD, 1.81) per person in the control group.
Subgroup analyses
Mobility improvement was greater for intervention participants who reported at least 45 minutes of baseline physical activity per week (adjusted mean difference, 2.7 [95% CI, 1.8–3.5] points) than for those who reported less (1.3 [95% CI, 0.3–2.3] points; P for interaction = 0.044). Sex, cognitive impairment, care type (home or residential aged care), and technology readiness did not influence differences between the intervention and control groups in the primary outcome (Box 7).
Implementation outcomes
Nine of twelve invited aged care service providers (75%) agreed to participate (adoption); 242 of 1348 people who received aged care from the participating service providers (18%) were screened, provided consent for participation, and participated in the trial, and 92 of 120 (77%) completed the six‐month program (reach). Intervention fidelity was good: intervention participants attended a mean 7.4 telephysiotherapy sessions (SD, 2.3 sessions) and 23 (SD, 4.9) of 26 support worker sessions. Based on exercise diaries, total mean exercise dose was 32.8 [SD, 17.7] hours (mean, 1.3 hours per week). One non‐injuring fall was reported (Box 8).
In post‐intervention surveys completed by 66 intervention participants (72%), the mean rating (scale, 1–10) for improvement in walking was 7.4 (SD, 1.7), in balance 7.5 (SD, 1.6), and fall risk reduction 7.0 (SD, 1.7). The mean rating for physiotherapy advice was 8.7 (SD, 1.3), the Zoom experience 8.1 (SD, 1.8), exercise videos 8.1 (SD, 1.3), and support worker engagement 9.2 (SD, 0.9). The overall rating for the TOP‐UP intervention was 7.8 (SD, 1.7) (Box 9); 62 people (94%) would recommend telephysiotherapy for other people.
Discussion
We report the first pragmatic randomised trial to evaluate a locally supported telehealth physiotherapist‐led program for improving mobility and preventing falls of people receiving aged care. TOP‐UP safely improved mobility in older people receiving aged care; its adoption, feasibility, and adherence were all good. Fewer intervention participants experienced falls during the program than control group participants. Sit‐to‐stand performance, balance, gait speed, mobility goal attainment, and quality of life also improved for intervention participants, and they reported reduced pain. Most intervention group participants would recommend the program to other people.
Mobility gains did not differ significantly by sex, cognitive impairment status, or care type (home or residential aged care), but were greater for participants who reported more baseline physical activity; however, clinically meaningful improvements were also achieved by participants who reported less baseline physical activity. The overall mean improvement in mobility score (2.1 points; 95% CI, 1.4–2.7 points) exceeded the thresholds for both the minimal clinically important difference (0.5 point) and for substantial change (1.0 point).31 The level of improvement achieved is associated with reduced risk of disability, institutionalisation, and mortality.34,35 Improved mobility may support functional recovery, including safer transfers, such as moving between bed and chair or between chairs, and greater independence in daily activities.23
Our findings are consistent with those of two effective in‐person, physiotherapist‐led group fall prevention programs for people in aged care in Australia: the Sunbeam trial3 and a dementia‐focused program.36 In the Sunbeam study, supervised strength and balance training using gym equipment was associated with a 55% reduction in the fall rate;3 the simpler, more readily expandable dementia‐focused program found a significant between–group difference in the falls rate during the intervention period.36 In the TOP‐UP program, participants received a mean 1.7 hours of exercise per week, similar to the other two programs, and this level may be sufficient for people receiving aged care. An update of the 2018 Cochrane review found that the fall reduction effects of physiotherapy programs are lost after interventions conclude,37 indicating that sustained exercise is needed. Telephysiotherapy could facilitate such exercise by providing ongoing remote access and care worker engagement.
The positive effects of TOP‐UP should be considered in the context of the broader telehealth literature. Physical benefits and cost savings are associated with telerehabilitation after knee replacement.38 Asynchronous telehealth is effective for the neurological rehabilitation of people with mobility limitations when adequate support is provided.39 Real‐time video‐based telerehabilitation achieves greater adherence and satisfaction than in‐person therapy, and is viable for older adults with mobility disabilities;40 it also fosters motivation and therapeutic relationships.41 Our qualitative findings suggest that the high acceptability of TOP‐UP is attributable to its accessibility, personalised care, and local support, which enhance motivation, self‐efficacy, and exercise independence.30
Limitations
The TOP‐UP trial was co‐designed with clinicians, older adults, and carers, and proved safe, effective, and acceptable, even for people with cognitive impairment and multiple medical conditions. However, the COVID‐19 pandemic slowed recruitment, and lockdowns may have influenced physical activity levels. Excluding people with severe cognitive impairment limits the generalisability of our findings. Relying on self‐reported participant information introduces recall bias. Support worker engagement probably varied, which could have affected the fidelity of intervention implementation. Recruitment of participants through aged care services may have favoured the participation of more engaged or better functioning older people. As intervention effects beyond six months were not measured, we cannot assess the longer term impact of our intervention. Digital literacy and technology‐related barriers were not comprehensively assessed, which may affect the generalisability of our findings to older people who have limited resources or are less comfortable with digital technology. We did not investigate the sustainability of the intervention program, workforce capacity, or system readiness.
Conclusion
Our TOP‐UP trial findings indicate that telephysiotherapy is a safe, effective, and expandable approach to improving the mobility of people receiving aged care, reducing falls risk and pain, and enhancing quality of life. The participants achieved clinically meaningful gains with high adherence to the program. The combination of telehealth, physiotherapy, and local support was effective, including for people with mild to moderate cognitive impairment. Our findings indicate that telephysiotherapy is a viable alternative that could be integrated into aged care when in‐person care is limited.
Box 1 – Selection of participants for the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023
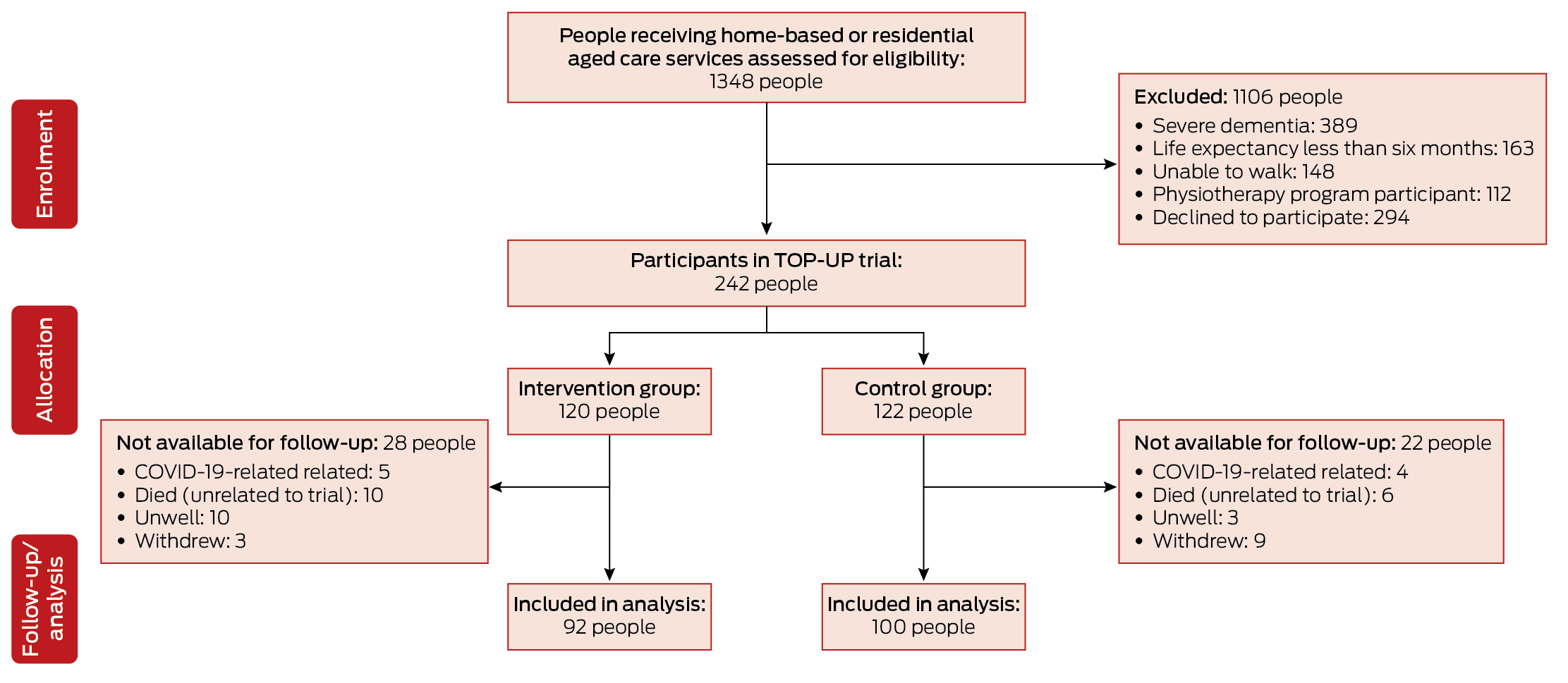
COVID‐19 = coronavirus disease 2019.
Box 2 – Baseline characteristics of participants in the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023
|
Characteristic |
Intervention group |
Control group |
All participants |
||||||||||||
|
|
|||||||||||||||
|
Participants |
120 |
122 |
242 |
||||||||||||
|
Age (years), mean (SD) |
83.2 (7.6) |
81.8 (8.2) |
83 (8) |
||||||||||||
|
Sex (women) |
78 (65%) |
80 (66%) |
158 (65%) |
||||||||||||
|
Care type |
|
|
|
||||||||||||
|
Residential aged care service |
51 (43%) |
52 (43%) |
103 (43%) |
||||||||||||
|
Home aged care service |
58 (48%) |
58 (47%) |
116 (50%) |
||||||||||||
|
Commonwealth Home Support service |
11 (9%) |
12 (10%) |
23 (7%) |
||||||||||||
|
Remoteness32 |
|
|
|
||||||||||||
|
Metropolitan |
73 (61%) |
75 (61%) |
148 (61%) |
||||||||||||
|
Rural |
41 (34%) |
41 (34%) |
82 (35%) |
||||||||||||
|
Remote |
6 (5%) |
6 (5%) |
12 (4%) |
||||||||||||
|
Country of birth |
|
|
|
||||||||||||
|
Australia |
85 (71%) |
90 (74%) |
175 (72%) |
||||||||||||
|
Other |
35 (29%) |
32 (26%) |
67 (28%) |
||||||||||||
|
Cognitive impairment |
|
|
|
||||||||||||
|
Telephone Interview for Cognitive Status score (0–41), mean (SD) |
28.7 (7.3) |
28.3 (6.6) |
29 (7) |
||||||||||||
|
No cognitive impairment |
60 (51%) |
69 (58%) |
129 (54%) |
||||||||||||
|
Mild cognitive impairment |
42 (35%) |
34 (29%) |
76 (31%) |
||||||||||||
|
Moderate cognitive impairment |
16 (14%) |
16 (13%) |
32 (13%) |
||||||||||||
|
Functional Comorbidity Index score,33 mean (SD) |
6.0 (2.5) |
5.8 (2.5) |
6 (2.5) |
||||||||||||
|
Pain score (visual analogue scale; 0–10), mean (SD) |
4.0 (3.1) |
4.0 (2.9) |
4 (3.0) |
||||||||||||
|
At least one fall during the preceding twelve months |
64 (53%) |
57 (47%) |
121 (50%) |
||||||||||||
|
Self‐reported balance (0–5), mean (SD) |
2.2 (1.0) |
2.2 (1.1) |
2.2 (1.0) |
||||||||||||
|
Self‐reported fear of falling (0–5), mean (SD) |
3.4 (1.3) |
3.6 (1.1) |
3.5 (1.2) |
||||||||||||
|
Quality of life (EQ‐5D‐5L) score (0–100), mean (SD) |
65.4 (18.3) |
67.2 (19.5) |
66 (19) |
||||||||||||
|
Number of medications, mean (SD) |
7.7 (3.5) |
7.5 (4.6) |
8 (4.1) |
||||||||||||
|
Mobility |
|
|
|
||||||||||||
|
Independent |
76 (63%) |
75 (62%) |
151 (62%) |
||||||||||||
|
With supervision |
31 (26%) |
32 (26%) |
63 (26%) |
||||||||||||
|
With assistance |
13 (11%) |
15 (12%) |
28 (12%) |
||||||||||||
|
Walking aid |
|
|
|
||||||||||||
|
None |
37 (31%) |
41 (34%) |
78 (32%) |
||||||||||||
|
Walking stick |
12 (10%) |
17 (14%) |
29 (12%) |
||||||||||||
|
Frame |
71 (59%) |
64 (52%) |
135 (56%) |
||||||||||||
|
Technology |
|
|
|
||||||||||||
|
Technology Readiness Index score (0–5), mean (SD) |
2.1 (0.8) |
2.1 (0.8) |
2.1 (0.8) |
||||||||||||
|
Own device (eg, iPad) |
48 (40%) |
39 (32%) |
87 (36%) |
||||||||||||
|
Prior telehealth use |
24 (20%) |
27 (22%) |
51 (21%) |
||||||||||||
|
Physiotherapy sessions in the preceding week, mean (SD) |
0.5 (1.3) |
0.5 (1.2) |
0.5 (1.2) |
||||||||||||
|
Planned exercise hours in the preceding week, mean (SD) |
1.2 (1.8) |
1.7 (2.5) |
1.5 (2.2) |
||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. |
|||||||||||||||
Box 3 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: intervention effectiveness
|
|
Control group |
Intervention group |
Intervention v control: adjusted between group difference (95% CI) |
||||||||||||
|
Outcome |
Baseline |
Six months |
Baseline |
Six months |
|||||||||||
|
|
|||||||||||||||
|
Participants |
122 |
100 |
120 |
92 |
|
||||||||||
|
Primary outcome (mobility) |
|
|
|
|
|
||||||||||
|
Short Physical Performance Battery (0–12), mean (SD) |
5.8 (2.9) |
5.6 (3.2) |
4.9 (2.9) |
7.2 (3.1) |
2.1 (1.4 to 2.7)* |
||||||||||
|
Secondary outcomes |
|
|
|
|
|
||||||||||
|
Sit‐to‐stand score (ordinal: 0–4), mean (SD) |
1.1 (1.2) |
1.1 (1.3) |
0.9 (1.2) |
1.4 (1.5) |
2.7 (1.3–4.3)† |
||||||||||
|
Sit‐to‐stand (continuous: seconds), mean (SD) |
24.7 (22.4) |
22.9 (12.2) |
23.4 (14.6) |
20.8 (12.3) |
–1.7 (–5.1 to 1.6)* |
||||||||||
|
Balance score (ordinal: 0–4), mean (SD) |
2.4 (1.3) |
2.0 (1.3) |
2.0 (1.3) |
3.0 (1.1) |
7.3 (3.6–14.7)† |
||||||||||
|
Balance (continuous), mean (SD) |
19.8 (9.2) |
18.5 (8.9) |
17.6 (8.8) |
24.3 (7.5) |
6.4 (4.3 to 8.5)* |
||||||||||
|
Gait speed score (ordinal: 0–4), mean (SD) |
2.3 (1.0) |
2.5 (1.2) |
2.0 (1.0) |
2.8 (1.2) |
1.9 (1.1–3.5)† |
||||||||||
|
Gait speed (continuous: seconds for 2.4 m), mean (SD) |
5.6 (3.5) |
5.5 (3.4) |
6.8 (8.3) |
4.8 (2.9) |
–0.9 (–1.6 to –0.1)* |
||||||||||
|
Mobility goal attainment (ordinal: –2 to +2), mean (SD) |
— |
–1.8 (0.7) |
— |
–0.2 (1.3) |
21.9 (10.7 to 44.8)* |
||||||||||
|
Goal met (dichotomous)‡ |
— |
3 (3%) |
— |
28 (30%) |
14.1 (4.1–48.5)† |
||||||||||
|
Pain (continuous: 0–10), mean (SD) |
4.0 (2.9) |
3.9 (3.1) |
4.0 (3.1) |
2.9 (3.0) |
–1.1 (–1.8 to –0.3)* |
||||||||||
|
Pain (dichotomous)§ |
— |
10 (10%) |
— |
17 (19.5%) |
2.0 (0.9–4.7)† |
||||||||||
|
Planned exercise (continuous: hours/week), mean (SD) |
1.7 (2.5) |
1.2 (1.6) |
1.2 (1.8) |
2.9 (2.7) |
1.7 (1.1 to 2.3)* |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; SD = standard deviation. * Adjusted mean difference: linear regression adjusted for baseline scores. † Adjusted odds ratio: logistic regression adjusted for baseline for dichotomous outcomes; ordinal regression adjusted for baseline for ordinal outcomes. ‡ Participants who met their mobility goal (ie, Goal Attainment Scale: 0 = met, +1 = better than goal, +2 = much better). § Participants who reported experiencing pain at baseline but not at follow‐up. |
|||||||||||||||
Box 4 – Mobility (Short Performance Physical Battery, SPPB) scores at baseline and six‐month follow‐up: mean values (with standard deviations), by participant study group
Box 5 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: quality of life
|
|
Control group |
Intervention group |
Intervention v control: adjusted between‐group difference (95% CI) |
||||||||||||
|
Outcome |
Baseline |
Six months |
Baseline |
Six months |
|||||||||||
|
|
|||||||||||||||
|
Participants |
122 |
100 |
120 |
92 |
|
||||||||||
|
EQ‐5D‐5L visual analogue scale (continuous: 0–100), mean (SD) |
67.2 (19.5) |
64.6 (17.6) |
65.4 (18.3) |
69.8 (16.4) |
6.2 (1.8 to 10.7)* |
||||||||||
|
Change in quality of life (ordinal: –2 to +2), mean (SD) |
– |
–0.3 (0.6) |
– |
1.0 (1.0) |
8.1 (3.4 to 10.0)† |
||||||||||
|
Improved quality of life (self‐report: dichotomous) |
– |
13 (13%) |
– |
47 (51%) |
7.0 (3.4–14.2)† |
||||||||||
|
Balance confidence (ordinal: 1–5‡), mean (SD) |
3.8 (1.0) |
4.0 (1.0) |
3.8 (1.1) |
3.4 (1.0) |
–0.3 (–0.2 to –0.5)† |
||||||||||
|
Fear of falling (ordinal: 1–5‡), mean (SD) |
2.4 (1.1) |
2.4 (1.2) |
2.5 (1.2) |
2.4 (1.2) |
–0.5 (–0.3 to –0.5)† |
||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; SD = standard deviation. * Units, based on linear regression model, adjusted for baseline. † Adjusted odds ratio: logistic regression adjusted for baseline for dichotomous outcomes; ordinal regression adjusted for baseline for ordinal outcomes. ‡ Lower numbers are better. |
|||||||||||||||
Box 6 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: falls
|
Outcomes |
Control |
Intervention |
Intervention v control: adjusted between‐group difference (95% CI) |
||||||||||||
|
|
|||||||||||||||
|
Participants |
100 |
192 |
|
||||||||||||
|
Falls |
96 |
58 |
IRR, 0.60 (0.35–1.01) |
||||||||||||
|
Participants with at least one fall |
44 (44%) |
29 (32%) |
RR, 0.62 (0.42–0.92) |
||||||||||||
|
Fall‐related fractures |
4 |
2 |
IRR, 0.51 (0.09–2.55) |
||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval; IRR = incidence rate ratio; RR = relative risk; SD = standard deviation. |
|||||||||||||||
Box 7 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: mobility (Short Performance Physical Battery) score, subgroup analyses
|
Characteristic |
Mean difference (95% CI) |
||||||||||||||
|
|
|||||||||||||||
|
Sex |
|
||||||||||||||
|
Women |
1.9 (1.1–2.7) |
||||||||||||||
|
Men |
2.4 (1.3–3.5) |
||||||||||||||
|
Cognitive impairment |
|
||||||||||||||
|
None |
1.9 (1.1–2.7) |
||||||||||||||
|
Mild/moderate |
2.4 (1.3–3.5) |
||||||||||||||
|
Care type |
|
||||||||||||||
|
Residential aged care facility |
2.0 (1.0–3.0) |
||||||||||||||
|
Home care service |
2.2 (1.1–2.7) |
||||||||||||||
|
Baseline physical activity* |
|
||||||||||||||
|
Less than 45 minutes |
1.3 (0.3–2.3) |
||||||||||||||
|
45 minutes or more |
2.7 (1.8–3.5) |
||||||||||||||
|
Technology Readiness Index score |
|
||||||||||||||
|
Less than 2 points |
2.1 (1.1–3.0) |
||||||||||||||
|
2–5 points |
2.0 (1.1–2.9) |
||||||||||||||
|
|
|||||||||||||||
|
CI = confidence interval. * Difference between categories: P = 0.044. |
|||||||||||||||
Box 8 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: implementation
|
Outcome |
Value |
||||||||||||||
|
|
|||||||||||||||
|
Adoption |
|
||||||||||||||
|
Aged care service providers participating in trial |
9/12 (75%) |
||||||||||||||
|
Reach |
|
||||||||||||||
|
Aged care recipients screened, provided consent, and participated in intervention |
242/1348 (18%) |
||||||||||||||
|
Fidelity |
|
||||||||||||||
|
Zoom physiotherapy sessions (maximum: ten), mean (SD) |
7.4 (2.3) |
||||||||||||||
|
Individual support worker sessions (maximum: 26), mean (SD) |
23.8 (4.9) |
||||||||||||||
|
Participants who completed the 6‐month intervention |
92/120 (77%)* |
||||||||||||||
|
Dose delivered |
|
||||||||||||||
|
Exercise quantity over six months (hours), mean (SD) |
32.8 (17.7) |
||||||||||||||
|
Safety |
|
||||||||||||||
|
Adverse events (falls and adverse musculoskeletal pain directly related to intervention) |
One non‐injuring fall |
||||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. * Twenty‐eight intervention participants who withdrew from trial were excluded from implementation outcome analysis: COVID‐19‐related illness, five; other illness, ten; dissatisfaction with the intervention, three; and ten participants had died. |
|||||||||||||||
Box 9 – Six‐month outcomes of the Telephysiotherapy for Older People (TOP‐UP) trial, 1 September 2021 – 30 November 2023: acceptability, based on survey responses of 66 intervention group participants
|
Question* |
Mean score (SD) |
Score range |
|||||||||||||
|
|
|||||||||||||||
|
Did TOP‐UP help your walking? |
7.4 (1.7) |
5–10 |
|||||||||||||
|
Did TOP‐UP help your balance? |
7.5 (1.6) |
5–10 |
|||||||||||||
|
Did TOP‐UP help your risk of falling? |
7.0 (1.7) |
2–10 |
|||||||||||||
|
How would you rate the physiotherapy advice using telehealth? |
8.7 (1.3) |
5–10 |
|||||||||||||
|
How would you rate your experience using Zoom? |
8.1 (1.8) |
4–10 |
|||||||||||||
|
How would you rate your experience using the exercise videos? |
8.1 (1.6) |
4–10 |
|||||||||||||
|
How would you rate your experience working with your coach? |
9.2 (0.9) |
7–10 |
|||||||||||||
|
How would you rate the TOP‐UP program overall? |
7.8 (1.7) |
2–10 |
|||||||||||||
|
|
|||||||||||||||
|
SD = standard deviation. * Likert scale: 0 = lowest rating; 10 = highest rating. |
|||||||||||||||
Received 8 November 2024, accepted 30 June 2025
- Rik Dawson1,2
- Marina Pinheiro1,2
- Juliana Oliveira1,3
- Abby Haynes1,2
- Vasikaran Naganathan1,2
- Morag E Taylor4,5
- Nina Bowes6
- Karn Nelson7
- Jenny Rayner1,2
- Catherine Sherrington1,2
- 1 The University of Sydney, Sydney, NSW
- 2 Sydney Local Health District, Sydney, NSW
- 3 Gold Coast University Hospital, Gold Coast, QLD
- 4 The University of New South Wales, Sydney, NSW
- 5 Neuroscience Research Australia, Sydney, NSW
- 6 Uniting AgeWell, Melbourne, VIC
- 7 Whiddon Group, Sydney, NSW
Open access:
Open access publishing facilitated by the University of Sydney, as part of the Wiley – the University of Sydney agreement via the Council of Australian University Librarians.
Data Sharing:
The data sets generated during this study are not publicly available because of the confidentiality promised to the participants as part of the informed consent process. However, data sets are available from the corresponding author upon reasonable request.
This trial was supported by research grants from Dementia Australia and Aged Care Research and Industry Innovation Australia (R2GA00007). The funders and organisations had no role in the trial design and did not have any role during its execution, analyses, interpretation of the data, or decision to submit the results. We thank Whiddon, Uniting AgeWell, Anglicare, Twilight, Ashfield Baptist Homes, and Maranatha House for their support. Rik Dawson received scholarship funding and Juliana Oliveria received salary support from the National Health and Medical Research Council‐funded Centre for Research Excellence—Prevention of Fall‐related Injuries (APP1198371). Marina Pinheiro holds a National Health and Medical Research Council of Australia Early Career Fellowship (GNT1156291).
Karn Nelson is employed by Whiddon. Nina Bowes is employed by Uniting AgeWell.
- 1. Eagar K, Westera A, Snoek M, et al. How Australian residential aged care staffing levels compare with international and national benchmarks. Centre for Health Service Development, Australian Health Services Research Institute, University of Wollongong, 2019. https://ro.uow.edu.au/articles/report/How_Australian_residential_aged_care_staffing_levels_compare_with_international_and_national_benchmarks/27702252?file=50445498 (viewed Jan 2022).
- 2. Bull FC, Al‐Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020; 54: 1451‐1462.
- 3. Hewitt J, Goodall S, Clemson L, et al. Progressive resistance and balance training for falls prevention in long‐term residential aged care: a cluster randomized trial of the Sunbeam program. J Am Med Dir Assoc 2018; 19: 361‐369.
- 4. Cameron ID, Dyer SM, Panagoda CE, et al. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst Rev 2018; 1: CD005465.
- 5. Dawson R, Suen J, Sherrington C, et al. Effective fall prevention exercise in residential aged care: an intervention component analysis from an updated systematic review. Br J Sports Med 2024; 58: 641‐648.
- 6. Royal Commission into Aged Care Quality and Safety. Final report: Care, dignity and respect. Volume 1: Summary and recommendations. 1 Mar 2021. https://www.royalcommission.gov.au/system/files/2024‐03/aged‐care‐rc‐final‐report‐volume‐1.pdf (viewed Jan 2022).
- 7. Eagar K, Westera A, Kobel C. Australian residential aged care is understaffed. Med J Aust 2020; 212: 507‐508. https://www.mja.com.au/journal/2020/212/11/australian‐residential‐aged‐care‐understaffed
- 8. Williams E, D’Amore W, McMeeken J. Physiotherapy in rural and regional Australia. Aust J Rural Health 2007; 15: 380‐386.
- 9. Eager K, Gordon R, Snoek M, et al. The Australian National Aged Care Classification (AN‐ ACC): a new casemix classification for residential aged care. Med J Aust 2020; 213: 359‐363. https://www.mja.com.au/journal/2020/213/8/australian‐national‐aged‐care‐classification‐acc‐new‐casemix‐classification
- 10. World Health Organization. WHO‐ITU global standard for accessibility for telehealth services. 1 Jan 2022. https://www.who.int/publications/i/item/9789240050464 (viewed Jan 2023).
- 11. Fisk M, Livingstone A, Pit SW. Telehealth in the context of COVID‐19: changing perspectives in Australia, the United Kingdom, and the United States. J Med Internet Res 2020; 22: e19264.
- 12. Dawson R, Oliveira JS, Kwok WS, et al. Exercise interventions delivered through telehealth to improve physical functioning for older people with frailty, cognitive, or mobility disability: a systematic review and meta‐analysis. Telemed J E Health 2024; 30: 940‐950.
- 13. Dawson R, Pinheiro M, Nagathan V, et al. Physiotherapy‐led telehealth and exercise intervention to improve mobility in older people receiving aged care services (TOP‐UP): protocol for a randomised controlled type 1 hybrid effectiveness–implementation trial. BMJ Nutr Prev Health 2023; 6: 273‐281.
- 14. Schulz KF, Altman DG, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 2010; 7: e1000251.
- 15. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014; 348: g1687.
- 16. Slade SC, Dionne CE, Underwood M, et al. Consensus on exercise reporting template (CERT): modified Delphi study. Phys Ther 2016; 96: 1514‐1524.
- 17. Ferrucci L, Del Lungo I, Guralnik J, et al. Is the telephone interview for cognitive status a valid alternative in persons who cannot be evaluated by the Mini Mental State Examination? Aging Clin Exp Res 1998; 10: 332‐338.
- 18. Parasuraman A, Colby CL. An updated and streamlined technology readiness index: TRI 2.0. J Serv Res 2015; 18: 59‐74.
- 19. Campbell AJ, Robertson MC, Gardner MM, et al. Randomised controlled trial of a general practice programme of home‐based exercise to prevent falls in elderly women. BMJ 1997; 315: 1065‐1069.
- 20. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377‐381.
- 21. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011; 6: 42.
- 22. Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81‐95.
- 23. Sherrington C, Lord SR, Vogler C, et al. A post‐hospital home exercise program improved mobility but increased falls in older people: a randomised controlled trial. PLoS One 2014; 9: e104412.
- 24. Boonstra A, Reneman M, Posthumus J, et al. Reliability of the life satisfaction questionnaire to assess patients with chronic musculoskeletal pain. Int J Rehabil Res 2008; 31: 181‐183.
- 25. Kolip P, Schaefer I. Goal attainment scaling as a tool to enhance quality in community‐based health promotion. Int J Public Health 2013; 58: 633‐636.
- 26. Delbaere K, Hauer K, Lord SR. Evaluation of the incidental and planned activity questionnaire (IPEQ) for older people. Br J Sports Med 2010; 44: 1029‐1034.
- 27. Oppe M, Devlin NJ, van Hout B, et al. A program of methodological research to arrive at the new international EQ‐5D‐5L valuation protocol. Value Health 2014; 17: 445‐453.
- 28. Filiatrault J, Gauvin L, Fournier M, et al. Evidence of the psychometric qualities of a simplified version of the activities‐specific balance confidence scale for community‐dwelling seniors. Arch Phys Med Rehabil 2007; 88: 664‐672.
- 29. McKay H, Naylor PJ, Lau E, et al. Implementation and scale‐up of physical activity and behavioural nutrition interventions: an evaluation roadmap. Int J Behav Nutr Phys Act 2019; 16: 102.
- 30. Dawson R, Gilchrist H, Pinheiro M, et al. Experiences of older people, physiotherapists, and aged care staff in the TOP‐UP telephysiotherapy program: interview study of the TOP‐UP interventions. JMIR Aging 2024; 7: e53010.
- 31. Kwon S, Perera S, Pahor M, et al. What is a meaningful change in physical performance? Findings from a clinical trial in older people (the LIFE‐P study). J Nutr Health Aging 2009; 13: 538‐544.
- 32. Australian Bureau of Statistics. Remoteness structure. Australian Statistical Geography Standard (ASGS), edition 3: July 2021 – June 2026. 20 July 2021. https://www.abs.gov.au/statistics/standards/australian‐statistical‐geography‐standard‐asgs‐edition‐3/jul2021‐jun2026/remoteness‐structure (viewed Jan 2022).
- 33. Groll DL, To T, Bombardier C, Wright JG. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 2005; 58: 595‐602.
- 34. Guralnik JM, Ferrucci L, Simonsick EM, at al. Lower‐extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995; 332: 556‐562.
- 35. Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA 2011; 305: 50‐58.
- 36. Brett L, Stapley P, Meedya S, Traynor V. Effect of physical exercise on physical performance and fall incidents of individuals living with dementia in nursing homes: a randomized controlled trial. Physiother Theory Pract 2021; 37: 38‐51.
- 37. Dyer SM, Suen J, Kwok WS, et al. Exercise for falls prevention in aged care: systematic review and trial endpoint meta‐analyses. Age Ageing 2023; 52: afad217.
- 38. Moffet H, Tousignant M, Nadeau S, et al. In‐home telerehabilitation compared with face‐to‐face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am 2015; 97: 1129‐1141.
- 39. Hassett L, van den Berg M, Lindley RI, et al. Digitally enabled aged care and neurological rehabilitation to enhance outcomes with activity and mobility using technology (AMOUNT) in Australia: a randomised controlled trial. PLoS Med 2020; 17: e1003029.
- 40. Simmich J, Ross MH, Russell T. Real‐time video telerehabilitation shows comparable satisfaction and similar or better attendance and adherence compared with in‐person physiotherapy: a systematic review. J Physiother 2024; 70: 181‐192.
- 41. Shulver W, Killington M, Morris C, Crotty M. “Well, if the kids can do it, I can do it”: older rehabilitation patients’ experiences of telerehabilitation. Health Expect 2017; 20: 120‐129.






Abstract
Objectives: To assess the effectiveness and implementation of a telephysiotherapy program for improving mobility, mobility goal attainment, and quality of life of people receiving at‐home or residential aged care.
Study design: Hybrid type 1 effectiveness–implementation randomised controlled trial.
Setting, participants: People aged 65 years or older who were receiving community or residential aged care services in Australia, 1 September 2021 – 30 November 2023.
Intervention: Telephysiotherapy for Older People (TOP‐UP): six‐month program of ten telephysiotherapy (Zoom) sessions for assessment and tailored exercise prescription, supported by trained aged care workers and exercise videos.
Main outcome measures: Primary outcome: mobility (Short Physical Performance Battery [SPPB] score at baseline and six months). Secondary outcomes: fall rate (per person), proportion of people with falls, SPPB components (sit‐to‐stand performance, balance, gait speed), pain (visual analogue scale), mobility goal attainment, physical activity (Incidental and Planned Exercise Questionnaire), quality of life (EQ‐5D‐5L visual analogue scale).
Results: A total of 1348 people were screened at 27 sites, and 242 eligible people were recruited for the trial (mean age, 83 years [standard deviation, 8 years]; 158 women [65%]); 92 of 120 intervention group participants and 100 of 122 control group participants completed the six‐month. After adjusting for baseline mobility scores, the mean difference in mobility score at six months (interventionv control group) was 2.1 (95% confidence interval [CI], 1.4–2.7) points. Sit‐to‐stand performance was more likely to improve in intervention than control participants (adjusted odds ratio, 2.7; 95% CI, 1.3–4.3); intervention participants reported greater quality of life (EQ‐5D‐5L visual analogue scale: adjusted mean difference, 6.2 [95% CI, 1.8–10.7] points) and less pain (visual analogue scale: adjusted mean difference, –1.1 [95% CI, –1.8 to –0.3] points), and a smaller proportion experienced falls (29, 32% v 44, 44%; risk ratio, 0.62; 95% CI, 0.42–0.92). Of 1348 screened people, 242 enrolled in the trial (18.0%), of whom 186 (77%) completed the trial, and 62 of 66 surveyed participants (94%) endorsed the intervention. No serious adverse events were recorded.
Conclusion: The TOP‐UP program safely improved mobility, reduced fall risk and pain, and improved quality of life for people receiving aged care. Telephysiotherapy could be incorporated into aged care to improve the lives of older Australians.
Trial registration: Australian New Zealand Clinical Trials Registry, ACTRN 12621000734864 (prospective).